KIPL Power Hour: International Physician Roundtable (6/26/2020)
This Power Hour features three Italian physicians who share their experiences of the COVID-19 pandemic.
KIPL Power Hour: Keeping Your Practice Afloat in Challenging Times (6/19/2020)
North Carolina physician owners and practice managers share lessons they have learned so far during the COVID-19 pandemic and detail what changes they have made in how they run their everyday procedures, workflows and finances.
Political Pulse for June 19, 2020
NCMS Director of Legislative Relations, Sue Ann Forrest, MPA, reveals that the end of session feels near, with lots of activity and a flurry of bills moving at the NC General Assembly. View this week's Political Pulse for all of the latest details.
Community Conversations: Harry Gallis, MD - A Broader Perspective on COVID-19 from an Infectious Disease Specialist

 Harry Gallis, MD, an infectious disease specialist and consulting professor in the Department of Medicine at Duke University, reflects on the history and changing environment and attitudes about infectious disease and what makes our current situation unique.
Harry Gallis, MD, an infectious disease specialist and consulting professor in the Department of Medicine at Duke University, reflects on the history and changing environment and attitudes about infectious disease and what makes our current situation unique.
Infectious diseases have been with us throughout human history – scientists have isolated various viruses in human tissue dating back hundreds, even thousands, of years. While our understanding of infectious diseases and how they spread has grown significantly, much remains unknown, as the current pandemic illustrates. Dr. Gallis has witnessed amazing scientific advances in his field, but also sees our enduring human limitations.
As an intern at Duke University in 1968, Dr. Gallis doesn’t recall any special training or attention paid to the flu, although that was the year of the Hong Kong influenza pandemic that killed millions of people worldwide. Several years later in 1971-72 as he moved on to his residency at Duke, he remembers seeing some otherwise healthy people coming into the emergency room with hypoxia. Several even died including a pregnant woman, which prompted some clinical changes.
“They decided that everybody coming into the emergency room who looked more than mildly ill had to get an arterial blood gas, and if their oxygen saturation was below a certain level, I think it was probably close to 90, they would be admitted for observation,” Dr. Gallis recalled. “But if you go back and look at that influenza season, nobody says anything about it. It just seemed to be a phenomenon related to our clinical practice at the time.”
A Cautionary Tale for Fast-Tracking a Vaccine
Five years later Duke’s Infectious Disease division was gaining traction, just in time for the swine flu epidemic. Public health officials at the time were fearful of a pandemic and they responded by fast- tracking a vaccine.
“They set goals to immunize over 200 million people against swine flu within six months,” Dr. Gallis said. “One of my classmates from medical school happened to be the special assistant to the Secretary of Health at the time, and he was the person who was put in charge of overseeing this program. When it went south, he was the one who caught the blame.”
[Del Meriweather, MD, MPH, US track and field champion and the first African-American student admitted to Duke University School of Medicine, was appointed Director of the US Public Health Service’s National Influenza Immunization Program (NIIP) in 1976. This program ultimately faced much opposition from doctors, pharmaceutical and insurance companies.]
While a direct link between this swine flu vaccine and the higher than usual incidence of Guillain-Barre syndrome among those vaccinated has never been definitively made, the public outcry prompted the government to call off the immunization program. Just over 22 percent of the population, had been immunized by the time the NIIP was stopped in December 1976.
“This has always been cited as one of the hazards of attempting to fast-track a vaccine,” Dr. Gallis said, noting the last coronavirus epidemics – SARS and MERS -- dissipated before there was even a thought of a vaccine. “The peculiar thing about this coronavirus [COVID-19] pandemic is that it is not going away, and the reasons are not entirely clear. Whether that has to do with the fact that it's much more contagious or more easily transmitted or that it persists in the air or on table tops or on peoples’ hands more than other coronaviruses have, we just don't know.”
Yet Dr. Gallis points out the incredible progress made in less than 50 years in this field. To illustrate this he recalls the mysterious outbreak of a pneumonia-like illness at a Legionnaires’ Convention in Philadelphia in 1976. It took 18 months to grow, isolate and identify this new bacterium, Legionella pneumophila, the cause of what’s now commonly called Legionnaires’ disease. To identify the virus causing HIV took two years. COVID-19 was genetically sequenced in a month.
“So that puts in perspective where we are in terms of the rapidity with which we diagnose and understand things in many ways. But in other ways, we don't right now know why this particular virus [COVID-19] appears to be more virulent and seems to have a higher mortality. We don't know the denominator. We don't know how many people out there are infected, compared to the number of people who get seriously ill compared to the number of people who die. So, to calculate true mortality statistics, we just don't know enough yet,” Dr. Gallis said.
Anecdotally, though, he knows mortality from COVID-19 is higher than the previous coronavirus outbreaks.
“When is the last time you saw somebody putting up temporary morgues outside of a hospital?” he asked. “That hasn't happened since 1918 that I'm aware of. Unless it was a catastrophic event like 911 or a plane crash.”
Beyond the Science
Beyond the scientific complexities making this pandemic unique, Dr. Gallis points to technology and politics as complicating factors. Social media has had positive impacts in getting necessary information out quickly, but along with the good information has come a wealth of misinformation, some of it harmful.
He also sees his former colleague at the National Institute of Allergy and Infectious Diseases, Anthony Fauci, MD, having to be more cognizant of politics as he seeks to manage the country’s response to the COVID-19 pandemic and keep science at the forefront.
“I think this is the first epidemic of this type that every turn and twist has been broadcast 24-7 by the media and has had the positive and negative interference of politics in it,” Dr. Gallis said. “When the decision was made to withhold United States funding from the World Health Organization, the Infectious Disease Society of America issued a statement that said, this is a bad mistake. This is going to harm the eradication of polio; it is going to harm the control of measles; it's going to harm all kinds of things that are going on in the world.
“Scientists are not respected anymore because of this stuff going on in the background, in the media, on the Internet where people are looking at information and believing whatever they see.”
Dr. Gallis feels Dr. Fauci should be the one delivering the media messages as the most respected infectious disease expert in the country today. His job is to oversee the appropriation and administration of infectious disease research dollars and that new information is appropriately based on the science, according to Dr. Gallis.
“Somehow or another, through information and knowledge, the facts have to begin to matter and prevail in this country again,” he said.
While Dr. Gallis admits this is the scariest time we’ve seen in a long time, he hopes that voters and elected officials will remember that we de-fund scientific research and institutions at our own peril.
“You know we're going to repeat this mistake again because that's what we do and that's a tragedy,” he said, pointing to the decades of coronavirus research by epidemiologist Ralph Baric, PhD at the University of North Carolina at Chapel Hill. People will ask, “Why are we giving that guy money?”
“This is why we're giving that guy money: because all of this matters, and it's going to continue to matter as human populations take over more previously unoccupied environments on this planet.”
If history does repeat itself in this case, it is likely that we will emerge from this pandemic with new knowledge, but hopefully with a longer lasting memory and the will to not repeat previous mistakes.
KIPL Power Hour: Future Clinician Leaders - A Conversation with Students (6/12/2020)
Future Clinician Leaders: A Conversation with Students on the Impact of COVID-19 on Their Education and Future
Medical students and residents share their views of – and any new revelations about – medicine, health care and leadership in light of their experiences during the COVID-19 pandemic.
KIPL Power Hour: Race and Health Equity (6/5/2020)
The events of the last few weeks have focused the nation’s attention on issues of racism and the many ways it is evident in our society. This week’s Power Hour brings together health care professionals who have thought profoundly about these issues and how they impact us, our patients and our communities. Please join us as we explore the current reality including discussion of health inequities and disparities, as well as what we can do as individual physicians, PAs and as part of an organization like the NCMS to foster positive change.
Participants include:
NCMS President Palmer Edwards, MD, DFAPA
NCMS Past President Paul R.G. Cunningham, MD
NCMS President-elect Philip M. Brown, Jr., MD
NCMS Strategy Officer Karen L. Smith, MD, FAAFP
NC Medical Board President Bryant A. Murphy, MD, MBA
George Pride, PhD, Founder, Black Doctors USA
Political Pulse for June 12, 2020
It was another busy week at the NC General Assembly. NCMS Director of Legislative Relations Sue Ann Forrest, MPA, highlights a new bill introduced because of the Covid-19 pandemic and shares the latest news on several bills that have moved forward in the legislative process.
KIPL Power Hour: Diabetes Prevention (5/29/2020)
More than 84 million Americans or 1 in 3 adults, has prediabetes and the majority of them don’t know they have it. Diabetes has reached epidemic proportions in the US. Left undetected and untreated, the progression to diabetes will continue to place a tremendous strain on physicians, clinical practices and health care costs associated with diabetes care and management. Through the statewide initiative in North Carolina to prevent type 2 diabetes called DiabetesFreeNC, physicians and care teams have an opportunity to support their prediabetic patients with a free or low cost evidence-based National Diabetes Prevention Program.
View a conversation where we will hear from Karen Smith, MD, and Brian Klausner, MD, as they share their thoughts and what actions they have taken to identify and manage their patients with prediabetes, including how they have managed their patients' health during the Covid-19 pandemic via telehealth, as well as how they have made referrals to various lifestyle change programs.
KIPL Power Hour: New Human Resource Challenges Arising during COVID-19 and How to Address Them (5/22/2020)
The COVID-19 pandemic has and continues to impact nearly every aspect of life as we know it. For health care employers, the working conditions have changed with the need to provide screening methods for both employees and patients, wear additional PPE, accommodate for social distancing etc. Additional modifications involve working in shifts, taking a pay cut, being furloughed and working from home only to mention a few. In a recent survey of the most pressing challenges for HR during COVID-19, 7 in 10 leaders cited crisis management or business continuity as their top challenge. This issue was closely followed by managing flexible work arrangements, managing employee communication, addressing employee concerns on workplace policies, implementation of preventive measures and reviewing current welfare policies.
Join us for conversation moderated by Franklin Walker, MBA, NCMS VP of Rural Health System Innovation, where we will hear from Kevin Ceglowski, JD, Kelsey Mayo, JD, and Steve Shaber, JD from Poyner Spruill about theses work-related challenges associated with the current national public health emergency and how to best address them.
KIPL Power Hour: NC Medical Board Response to COVID-19 (5/15/2020)
The NC Medical Board has taken many steps since March to support the state’s response to COVID-19. NCMB’s primary goals are to remove barriers and support physicians, physician assistants and the state’s health care system as a whole during this rapidly-evolving pandemic. How has NCMB responded to requests from Gov. Cooper, NC DHHS, health systems, licensees and member associations such as the NC Medical Society? What steps has NCMB taken to be more flexible and responsive during the current state of emergency?
Join a conversation moderated by Franklin Walker, MBA, NCMS VP of Rural Health Systems Innovation with speakers from the NC Medical Board: Bryant Murphy, MD, Board President; Thom Mansfield, JD, Chief Legal Officer; Evelyn Contre, Chief Communications Officer; and Marcus Jimison, Sr., JD, Staff Attorney.
Power Hour: Self-Care and Wellness during Covid-19 (5/8/2020)
There has been an increased attention to stress and burnout among clinicians for some time. However, this unprecedented time of pandemic worry puts a new spin on how stress affects us in our everyday lives and how we can address that. Join a conversation around self-care and wellness that includes talking about healthy habits but also goes beyond to talk about handling loss of control both personally and professionally. How does, for example, organizational culture impact our well-being and what do we do when we feel we cannot do anything?
Franklin Walker, MBA, NCMS VP of Rural Health Systems Innovation, will moderate the conversation that features Cormac O’Donovan, MD, and Marion McCrary, MD, who both have a passion for wellness and stress reduction. They will talk about their respective experiences and knowledge around this important topic.
NCMS Political Pulse for May 8, 2020
NCMS Director of Legislative Relations, Sue Ann Forrest, MPA, highlights a week that featured Gov. Roy Cooper sign two Covid-19 relief bills into law and an important NCMS member call take place with NC DHHS officials. Watch the video to get her synopsis.
Power Hour: A Specialist Perspective on COVID-19's Impact on Medical Practices (5/1/2020)
Hear from different specialty society leaders regarding how they've adapted their practices in the face of this pandemic. They will share the challenges they are facing as well as their thoughts on the future of their respective specialties. Moderated by Franklin Walker, MBA, NCMS VP of Rural Health Systems Innovation, this session will provide you an opportunity to listen to Craig Burkhart, MD and Susan Sanders, MD, both past presidents of the NC Dermatology Association; Sarah Koch, MD and Dhwani Mehta, MD from the Dermatology Group of the Carolinas; Janelle Rhyne, MD, a past Governor of the NC Chapter, American College of Physicians; and Gaurang Palikh, MD, President of the North Carolina Neurological Society.
NCMS & NCHA Task Force Offer Guidance on Re-Opening the Economy and Resuming Certain Health Services
Today the joint NCMS and NC Healthcare Association (NCHA) Task Force on Virus Mitigation in an Open Economy, which includes physicians from a variety of specialties and representatives from the NCHA, issued a media statement on resuming economic activity during the COVID-19 pandemic. Task force members emphasized the need, above all, to protect public health through continued social distancing and other efforts to slow the spread of the virus and recognized that a thoughtful and measured approach to resuming business activities is necessary. Read the media statement on reopening the economy.
The Task Force also agreed on another document outlining the principles for resuming health services during the pandemic. In drafting the principles, which are meant to broadly encompass surgical, specialty and primary care practices, the task force was adamant that patients are the top priority in considering how to move forward and resume time-sensitive procedures or treatments.
“Patients should be triaged for priority and a standard of medical necessity must be applied before each service,” the document states and goes on to outline considerations such as having adequate supplies of personal protective equipment and other resources available before resuming such treatment.
The Task Force also was highly aware that these decisions must be made at the local level.
“The specific approach to restarting and continuing to perform such services is most appropriately developed and implemented at the health care community or region level, taking into account the extent of COVID-19 disease in the region and any resource constraints within facilities,” the document states.
Read the “Principles for Health Services During Covid-19 Pandemic” here.
Also today, Governor Roy Cooper outlined a phased approach to gradually loosening his stay-at-home order, possibly allowing more businesses to reopen starting May 9. In order to move to the first phase in lifting some of the current restrictions, data trends outlined by NC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH, must show declines or sustained leveling in the number of COVID-19 cases and other metrics. The state must also have at least 30 days of testing and PPE capacity to safely begin the process, she said. Here are the slides from the Governor and Secretary Cohen’s presentation, which outline each of the metrics the state will use to determine lifting restrictions.
Power Hour: Stress in the Time of COVID-19 (4/17/2020)
View a chat around the mental health aspects of working in health care during these times and what issues people are dealing with. Moderated by Franklin Walker, MBA, VP Rural Health Systems Innovation and Harold Kudler, MD, Adjunct Associate Professor in the Department of Psychiatry and Behavioral Sciences at Duke University School of Medicine, you will have the opportunity to listen to Zach Feldman, MD, NC Psychiatric Association President Elect; Therese Garrett, MD, President of the NC Council of Child & Adolescent Psychiatrists; and Nkechi Conteh, fourth year adult psychiatry resident, about the behaviors we notice around us and how we can handle those. This Power House video is an opportunity to learn from each other about the impact of a pandemic on our behavior and stress levels and to think about how we can integrate our perspectives to achieve better outcomes for our patients and for ourselves and our families.
Financial Guidance from Smith Anderson Amid Covid-19 Crisis
NCMS’ partner Smith Anderson held a call to review the various financial options available to you and your practice. We recorded the call so you can tap into the information provided. Listen below.
https://www.ncmedsoc.org/smith-anderson_040620_financial-help/
Robert Shaw, chair of Smith Anderson's health care practice, and Peter Bosman, a partner in Smith Anderson’s Private Equity group, reviewed the menu of financial options provided thus far by the federal government and offered some strategic considerations as you may weigh the various programs. Topics covered in the hour-long call, in the following order, included:
- An overview of the CARES Act and its two provisions of most interest to small businesses, the Paycheck Protection Program and the Economic Injury Disaster Loan Program (EIDL).
- Payroll tax credits.
- Medicare accelerated or advance payments and what private insurers are doing in this area. They also discussed the NC Department of Insurance and their ‘strongly worded encouragement’ to insurers to defer premium payment requirements to help ensure there is no lapse in coverage for beneficiaries.
- The distinctions between permanent and temporary layoffs of staff and furloughs.
- Obligations if you need to close your practice.
- The Family First Act and its provisions.
Shaw and Bosman also answered questions submitted before the call. If you have a follow up question, you may email it to [email protected]. Watch for details on future calls to address other financial topics of concern to NCMS members as you respond to the economic impact of the COVID-19 pandemic.
Power Hour: Telehealth (4/3/2020)
Originally created as a way to reach patients remotely, telehealth needs during the COVID-19 pandemic have skyrocketed. Physician practices are working to get telehealth platforms set up and running so they can continue to see patients. This Power Hour is an opportunity to share knowledge and learn from each other about applying telehealth technology during this pandemic. Steve North, MD, a family physician and adolescent medicine specialist in Mitchell County, Reynold Yordy, who has 20 years of health care IT and programming experience and the NCMS’ Vice President for Rural Health Systems Innovation Franklin Walker lead the conversation.
Webinar: Integrating Telehealth Into Your Practice in a Pandemic & Beyond - Thurs., April 9
The North Carolina Medical Society Foundation is pleased to offer this free webinar on telehealth integration featuring Steve North, MD, MPH, FAAFP, State Medical Director for Eleanor Health
Thursday, April 9, 2020 | 1:00 pm to 2:00 pm
Register here:
https://attendee.gotowebinar.com/register/2028822560038297869
This webinar is free but you must be registered to attend. Space is limited so register early!
After you register, you will receive an emailed confirmation with webinar and phone-in instructions.
About Steve North, MD, MPH, FAAFP:
 Dr. North is the State Medical Director for Eleanor Health and a practicing Family Physician and Adolescent Medicine specialist at a rural health center in Mitchell County, NC.
Dr. North is the State Medical Director for Eleanor Health and a practicing Family Physician and Adolescent Medicine specialist at a rural health center in Mitchell County, NC.
In 2011, he founded the Health-e-Schools school-based telemedicine program that currently provides access to acute care, primary care, adolescent medicine, and comprehensive asthma services to over 35,000 students at 80 schools in six school districts across North Carolina. In 2014 the Health-e-Schools program was awarded the American Telemedicine Association’s President’s Award for Health, Quality and Innovation.
He served as the Medical Director for Mission Virtual Care from 2014-2019 working with a team to integrate inpatient, outpatient, virtual visits, and remote home monitoring into Mission Health, North Carolina’s sixth largest health system that serves the state’s 18 western most counties.
Dr. North is the Rural Telehealth Research Fellow at the University of North Carolina’s Sheps Center for Health Services Research, a member of the HRSA Rural Telehealth Research Center, leads the SPROUT school-based research interest group, and was a member of the National Quality Forum’s Telehealth Committee. He currently serves on the boards of the Mid-Atlantic Telehealth Resource Center and the Foundation for Health Leadership and Innovation and, is a co-author of the American Telemedicine Association’s Operating Procedures for Pediatric Telehealth and the Practice Guidelines for Telemental Health with Children and Adolescents.
NCMS Offers Telemedicine Help Through New Platform "Presence"
In response to the COVID-19 pandemic and in an effort to ease the burden on North Carolina’s physicians and patients, the NCMS today is launching a telemedicine platform available to all health care providers in North Carolina at no charge, until the COVID-19 pandemic abates. This custom platform, called Presence, was produced in a collaboration between the NCMS Foundation’s Project OBOT NC and The Recovery Platform.
The Presence platform provides a central portal where patients can schedule a telemedicine visit with their provider. In fact, patients can look up their provider by practice or provider name and are given a calendar with times the physician has reserved for telemedicine or phone based appointments. Physicians will receive a notification of scheduled visits and access the Presence dashboard to initiate and manage these patient interactions.
To setup your account you simply need to:
• Go to the onboarding page here.
• Activate your account to setup your Telemedicine Availability Schedule
• Login to the dashboard to see upcoming scheduled visits
• Initiate the patient visit
• Digitally order labs on the platform with our integrated partners
• Charting and billing are performed in your own EHR
After you receive confirmation your account is set-up you will be provided with instructions to:
• Sign the BAA
• Download Zoom at https://zoom.us/download
• Email patient roster (suggested language below)
Learn more about Presence and how you can access this valuable NCMS Foundation resource
Covid-19 News and Updates
Keeping up with Covid-19: Latest Info for NC Health Care Professionals
Remember: The most timely and credible information is available at the
|
Covid-19 Testing guidance
To facilitate greater access to testing for the virus that causes Covid-19, NCDHHS is encouraging providers to submit specimens to LabCorp when ALL of the following conditions are met:
• Fever
• Signs/symptoms of lower respiratory illness (e.g., cough, shortness of breath)
• Negative influenza test (rapid or PCR).
Guidance for testing at LabCorp is available here.
Here is the latest NCDHHS testing guidance.
Clinicians should use their judgment to determine which patients are most in need of testing. NCDHHS does not recommend testing of asymptomatic patients for COVID-19.
Read the memo from NCDHHS on testing through LabCorp.
Personal Protective Equipment Guidance
For the latest on Personal Protective Equipment recommendations, visit the CDC webpage here.
Reimbursement Guidance
While there is no code for Covid-19, utilization of the CDC recommended codes should lead to less questioning by commercial insurers like Blue Cross and Blue Shield of NC and a higher likelihood of payment. Here is the ICD-10 coding guidance from the CDC.
We’ve been hearing concerns about reimbursement for telehealth, testing and other issues arising from Covid-19. For NCMS member practices, the NCMS Plan has signed an amendment with Blue Cross and Blue Shield of NC covering COVID-19 testing.
Below is information from each of the major commercial insurance companies in the state and what they have provided thus far to their physicians and PAs.
Aetna
• Guidance on telehealth
• General clinical updates
Blue Cross and Blue Shield of NC
• Telehealth policy
Cigna
• Testing reimbursement
• Telehealth update
Humana
• Message for clinicians with resource links
• Telehealth guidance
United Healthcare
• General guidance
• Telehealth guidance
Medicare/Medicaid
On March 12, the Centers for Medicare and Medicaid Services (CMS) posted a fact sheet with information relating to the pricing of both the CDC and non-CDC tests.
CMS' Quarterly Update for Clinical Laboratory Fee Schedule and Laboratory Services Subject to Reasonable Charge Payment contains the latest information on Advanced Diagnostic Laboratory Tests, pricing and new codes. On page 3 of the update, the new COVID-19 codes are referenced.
Essential Health Benefits (EHB) Coverage
On March 12, CMS issued Frequently Asked Questions (FAQs) about EHB to ensure individuals, issuers and states have clear information on coverage benefits for COVID-19. This action is part of the broader, ongoing effort by the White House Coronavirus Task Force to ensure that all Americans – particularly those at high-risk of complications from the COVID-19 virus – have access to the health benefits that can help keep them healthy while helping to contain the spread of this disease.
For more information specific to CMS, please visit the Current Emergencies website.
The President’s declaration of a national emergency last week, empowers the Secretary of Health and Human Services (HHS) to take proactive steps through 1135 waivers to waive certain Medicare, Medicaid and Children’s Health Insurance Program (CHIP) program requirements and conditions of participation.
Waivers and Flexibilities for Hospitals and other Health Care Facilities: CMS will temporarily waive or modify certain Medicare, Medicaid and CHIP requirements. These waivers provide continued access to care for beneficiaries. Learn more.
Provider Enrollment Flexibilities: CMS will temporarily suspend certain Medicare enrollment screening requirements including site visits and fingerprinting for non-certified Part B suppliers, physicians and non-physician practitioners. In addition, CMS will allow licensed providers to render services outside their state of enrollment. CMS will also establish a toll-free hotline for providers to enroll and receive temporary Medicare billing privileges.
Flexibility and Relief for State Medicaid Agencies: The national emergency declaration also enables CMS to grant state and territorial Medicaid agencies a wider range of flexibilities, which are outlined in the Medicaid and CHIP Disaster Response Toolkit. Examples of flexibilities available to states include the ability to permit out-of-state providers to render services, temporarily suspend certain provider enrollment and revalidation requirements to promote access to care, allow providers to provide care in alternative settings, waive prior authorization requirements and temporarily suspend certain pre-admission and annual screenings for nursing home residents.
Get more information and to access the toolkit.
Suspension of Enforcement Activities: CMS will temporarily suspend non-emergency survey inspections, allowing providers to focus on the most current serious health and safety threats, like infectious diseases and abuse.
CMS hosted two webinars in 2018 regarding Emergency Preparedness (EP) requirements and provider expectations including emergency power supply, the 1135 waiver process, best practices and lessons learned from past disasters, helpful resources and more. Watch those webinars.
Access information on NC Medicaid fee schedules here.
For questions, concerns or input on issues around NC Medicaid and Covid-19 use this email address:
Telehealth
To help protect patients and staff from spread of Covid-19 many practices are looking to telehealth technology.
NC Medicaid will allow practices to bill for defined telehealth services. Review the updated policies in this special NC Medicaid Bulletin.
Blue Cross and Blue Shield of NC has expanded Telehealth Measures effective March 6, 2020. Visits that previously required an in-person encounter can be performed virtually and will be paid at parity with office visits as long as they are medically necessary, meet criteria in the updated Blue Cross NC Telehealth Corporate Reimbursement Policy, and occur on or after March 6, 2020. They offer the following guidance:
- These temporary measures include virtual care encounters for patients that can replace in-person interactions across appropriate care settings, including outpatient clinics, hospitals, and the emergency departments.
- Please do not file telehealth claims with Blue Cross NC until March 21, 2020 and use Telehealth as Place of Service (02).
- For providers or members who don’t have access to secure video systems, telephone (audio-only) visits can be used for the virtual visit. Please use both Telehealth as Place of Service and CR (catastrophe/disaster-related) modifier for audio-only visits.
- If you believe an eligible telehealth claim has been improperly denied, please resubmit it after March 21, 2020.
- Some commercial members can access MDLIVE or TeleDoc as a virtual care benefit, as noted on their member ID card. Federal Employee Program (FEP) members can only access virtual care through the Teledoc service. Teledoc offers both video or audio virtual services. You can view COVID-19 benefits for the Federal Employee Program here.
Guidance to Providers Regarding Virtual Visits for Blue Cross NC Commercial and Medicare Advantage Members These measures will remain in effect for a 30-day period, starting March 6, 2020, and then be re-evaluated for extension.
If you are interested in learning more about how to implement telehealth into your practice, Curi, a Medical Mutual Company, offers this quick one-page summary offering guidance on the structure/execution of clinical telehealth services, as well as a number of links to resources and regulatory bodies. Curi Telehealth Overview.
Wake County Health Department Offers Help
The Wake County Health Department has compiled a list of Q&As to assist in getting the information health care professionals need about this evolving situation, while also providing a better understanding of public health’s role in working to contain this novel coronavirus. Access that list.
Some of the questions addressed in the FAQs include:
• What should I do with a patient who is exhibiting the symptoms associated with COVID-19?
• Who should be tested for COVID-19?
• What if one of my patients test positive for COVID-19?
• How can our office test for COVID-19?
• What is my risk to my staff and providers?
• Should I send patients that need COVID-19 testing to the Wake County Health Department for testing?
You can visit the Wake County Health Department's COVID-19 webpage, which has a set of frequently asked questions to educate providers. You can also email the department questions at [email protected], or you can call its COVID-19 information line at 919-856-7044. The county is also sharing important information on its Facebook, Twitter and Instagram accounts.
NC Medical Board Adopts Emergency Rules
The NC Medical Board (NCMB) and the NC Rules Review Commission have approved emergency rules allowing a physician or PA who inactivated his or her NC medical license within the past 24 months to quickly obtain a temporary license to support Gov. Roy Cooper’s declaration of a state of emergency due to Covid-19. The license would authorize the physician or PA to practice for 90 days or until the state of emergency in North Carolina is declared over. Read the rules.
Over the next few days, NCMB will develop an online application form to receive temporary license requests from interested physicians and PAs. We expect to have this application ready by sometime next week. NCMB is not currently accepting requests for the new temporary emergency license.
Issuance of temporary authority to practice is subject to the following conditions:
• The applicant must demonstrate that he or she has practiced clinical medicine for at least 80 hours during the most recent 24 months;
• The applicant must have been licensed continuously for at least 10 years prior to making his or her medical license inactive;
• The applicant must have no history of public discipline and must not have inactivated his or her license while under investigation; and
• The applicant must confine his or her practice to areas in which he or she is clinically competent.
Please note that the NCMB adopted the emergency rules to support the Governor’s declaration of a state of emergency, which identifies a need to develop additional medical resources in the state, including additional providers. This is a preparedness step – there’s no indication that there’s a current need for additional medical providers to assist with COVID-19.
NCMB will likely advise inactive physicians and PAs who may be interested in returning to practice to check in with their local public health departments, former employer/practice, local hospital or other health care employer to determine if they are needed.
For the most up-to-date information visit the NCMB website.
Other Resources
Toolkit for Independent Physicians
Thanks to our friends at Avance Care, who have shared this toolkit for independent practices grappling with their response to Covid-19. The kit includes practical advice and resources to protect staff; recommendations for room decontamination; sample scripts for patients who may demand testing even if it’s not warranted by clinical guidelines and links to other resources.
Hand hygiene videos
This New England Journal of Medicine video on hand hygiene is excellent and pretty technical. It's 14 minutes long.
For patients, this National Health Service hand hygiene video has no words, just a great demo and lasts just 44 second. has a that has no words, just a great demo, 44 seconds
CDC Hand Hygiene Fact Sheets and Posters
Provider Poster :Clean-Hands-Count
Poster Clean Hands Count For My Patients
Articles of interest
Coronavirus (Covid-19): New Telehealth Rules and Procedure Codes for Testing, FPM Journal, 3-10-20
CMS Announces Relief for Medicare Providers
The Centers for Medicare & Medicaid Services (CMS) has announced an expansion of its accelerated and advance payment program for Medicare participating health care providers and suppliers, to ensure they have the resources needed to combat the 2019 Novel Coronavirus (COVID-19). This program expansion includes changes that were part of the recently enacted Coronavirus Aid, Relief, and Economic Security (CARES) Act.
Accelerated and advance Medicare payments provide emergency funding and address cash flow issues based on historical payments when there is disruption in claims submission and/or claims processing. These expedited payments are typically offered in natural disasters to accelerate cash flow to the impacted health care providers and suppliers. In this situation, CMS is expanding the program for all Medicare providers throughout the country during the public health emergency related to COVID-19. The payments can be requested by hospitals, doctors, durable medical equipment suppliers and other Medicare Part A and Part B providers and suppliers.
To qualify for accelerated or advance payments, the provider or supplier must:
- Have billed Medicare for claims within 180 days immediately prior to the date of signature on the provider’s/ supplier’s request form,
- Not be in bankruptcy,
- Not be under active medical review or program integrity investigation, and
- Not have any outstanding delinquent Medicare overpayments.
Medicare will start accepting and processing the Accelerated/Advance Payment Requests immediately. CMS anticipates that the payments will be issued within seven days of the provider’s request.
An informational fact sheet on the accelerated/advance payment process and how to submit a request is available here.
NCMS Statement on Governor's Stay-at-Home Order
Governor Roy Cooper issued a statewide stay-at-home order this afternoon. Below is the NCMS' statement to the media in response to the order.
RALEIGH -- We applaud Governor Cooper’s decisive action today in issuing a statewide stay-at-home order. This is an historic public health crisis and Governor Cooper’s demonstrated leadership is crucial in protecting the people of North Carolina. We thank him for making this difficult decision, which we acknowledge will have far reaching impacts.
The NCMS, which advocates on behalf of physicians and PAs and their patients throughout the state, encouraged Gov. Cooper to increase the restrictions on non-essential public contact in order to stem the spread of COVID-19. Our leadership seriously weighed the consequences such a position would have on our communities -- both businesses and individuals. As medical professionals, sworn to protect the health of our patients, a stay-at-home order such as the Governor issued is warranted and necessary.
Being cognizant of the economic and mental health toll of this pandemic, today’s action will blunt the negative impact as much as possible. We are lobbying our state and federal officials to enact emergency economic policies to support small business – including medical practices – and the workforce, and we are developing a wealth of resources in consultation with our member mental health experts to offer emotional support during this difficult time.
We will be sharing more about how we are supporting our health care community and the larger public in media releases in the coming days.
NC DHHS Issues New Telepsychiatry/Telehealth Policy Guidance
Effective Monday, March 30, 2020, the NC Department of Health and Human Services (NCDHHS) is temporarily modifying enhanced behavioral health policies and telemedicine and telepsychiatry policies to better enable the delivery of remote care to Medicaid and state-funded beneficiaries during the COVID-19 outbreak. This will include dates of service on or after March 10, 2020 and will remain in effect until the State of Emergency is declared over or when this policy is rescinded.
Details on the temporary modifications are included in the following Special Bulletins:
- SPECIAL BULLETIN COVID-19 #19: Telehealth Provisions for Enhanced Behavioral Health Services
- SPECIAL BULLETIN COVID-19 #20: Update to Telehealth Provisions: Clinical Policy Modifications
Additional information on COVID-19 for Medicaid providers is available here.
NCMS To Testify This Morning Before NC Legislative Committee
NCMS Board of Directors At-Large member Eileen Raynor, MD, FACS, FAAP and NCMS Senior Vice President for Advocacy Chip Baggett, JD, will testify before the NC House Select Committee on COVID-19, which will be meeting virtually this morning at 10 a.m.
In this report, we offer legislators a comprehensive look at the current conditions in which physicians and PAs in North Carolina now find themselves. And we will present committee members with policy recommendations in hopes they will take action to help you do your job effectively during this historic event and to blunt its financial impact on those serving on the frontlines, like you.
Advocating for our members and protecting the public health always has been at the heart of the NCMS since its inception in 1849. Responding to the COVID-19 pandemic is just the latest example of how we mobilize our resources on behalf of physicians and PAs across North Carolina.
Read the report. You can listen in on the hearing live, today at 10 a.m. at this link.
NCMS Asks Governor To Increase Restrictions To Help Prevent Spread of COVID-19
Today, the North Carolina Medical Society (NCMS), representing physicians and PAs statewide, called on Governor Roy Cooper to enact an Executive Order to stop the public’s in-person access to non-essential businesses in order to limit community spread of the COVID-19 virus. The letter requests the more stringent restrictions be put in place for a two-week period in order for the Governor, in consultation with his team of public health and economic experts, to re-evaluate the effect of the order in that timeframe and make any necessary adjustments to benefit North Carolinians.
“We are acutely aware of the impact such an order will have on our state from an economic perspective and seriously weighed those considerations before making this request,” said NCMS President Palmer Edwards, MD, DFAPA. “As health care professionals, however, we felt it our duty to urge stronger protections for the public and our colleagues on the front lines in this pandemic.”
The letter notes the shortages of personal protective equipment many physicians and PAs currently are grappling with as they try to treat patients. It also applauds the Governor’s leadership thus far while calling on him to take decisive action now to help curb the spread of the virus.
“Since its founding in 1849, the NCMS has been dedicated to protecting the public health,” said NCMS CEO Robert W. Seligson, MBA, MA. “Today, our members are selflessly carrying forward those values and we look forward to continuing to work with our state’s leaders to help them serve the citizens of North Carolina during this latest public health crisis.”
Read the NCMS’ letter to Governor Cooper.
NCMS Mobilizing "Stay at Home" Campaign
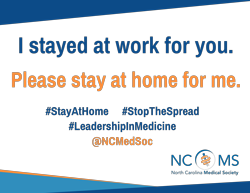 Join the #StayAtHome Campaign! In an effort to encourage people to stay at home to slow the spread of COVID-19, the NCMS is offering you a special message to put out on your social media channels as many other health care professionals are doing.
Join the #StayAtHome Campaign! In an effort to encourage people to stay at home to slow the spread of COVID-19, the NCMS is offering you a special message to put out on your social media channels as many other health care professionals are doing.
Just print out this “I stayed at work for you. Please stay at home for me” sign, take a picture of you and/or your staff holding it and send it out via Twitter, Facebook or Instagram. Be sure to tag @ncmedsoc.
This is one way to make sure the public is following the state and federal guidance about physically distancing themselves to slow the spread of the virus and to help protect physicians and PAs like you, who are on the frontlines treating those who are ill with non-Covid-19 related illnesses as well as those who are infected. You, our health care professionals, are our most valuable resource during this pandemic.
Thank you for all you do!
Finding Peace in a Time of Crisis
https://www.ncmedsoc.org/emotional-support-resources-for-health-care-teams-during-covid-19/
NCDHHS Calls for Medical Volunteers
The NC Department of Health and Human Services (NCDHHS) is asking for medical volunteers to “bolster our health care system to ensure we can care for those impacted by the Covid-19 virus. A crucial part of that effort is recruiting volunteers to supplement our health care workforce. We are asking for your help to meet these needs,” wrote NCDHHS Secretary Mandy Cohen, MD, MPH in a letter to health care organizations.
Read the full letter. (PDF)
The state is using an online platform called NC Training, Exercise, and Response Management System (NC TERMS) where physicians, PAs, nurses and other clinical support staff as well as non-clinical support staff can sign up to volunteer. The NC Medical Board will ensure licensure and the system will be used to direct medical staff where most needed. Get step-by-step instructions on how to create an account and sign up to volunteer on NCTERMS. (PDF)
According to NC General Statute 166A individuals providing health care services as part of a State Medical Assistance Team designated by the North Carolina Office of Emergency Medical Services will be considered an “emergency management worker” and will be subject to the Immunity and Liability provisions outlined in 166A-19.60, according to the letter.
Political Pulse for March 20, 2020
Thank You! NCMS Senior VP for Advocacy and Advancement Chip Baggett, JD, wants to thank you for the selfless work you are doing to keep our communities safe and healthy. And he describes how the NCMS is working behind the scenes to help ensure collaboration and coordination with state and federal agencies and promote legislation protecting you and your practice. He also reminds you to be sure to take care of yourself during these stressful times. The NCMS is developing tools to help.
NC 2-1-1 to Provide Assistance for COVID-19
Governor Roy Cooper announced NC 2-1-1 by United Way of North Carolina as a resource for people to call for assistance related to the COVID-19 coronavirus.
North Carolinians can text COVIDNC to 898211 to receive general information and updates about COVID-19. Sign up now to get regular alerts on the rapidly evolving situation and North Carolina’s response.
NC 2-1-1 can refer callers to the organizations in their local community best equipped to address their specific health and human services needs including food, shelter, energy assistance, housing, parenting resources, health care, employment, substance abuse treatment, as well as specific resources for older adults and for persons with disabilities, and much more. Simply dial 2-1-1 or TTY 888-892-1162 for assistance.
All North Carolinians are encouraged to visit www.ncdhhs.gov/coronavirus for reliable, up-to-date information. Included on this page is helpful information for:
- Individuals and Families
- Businesses and Employers
- Providers
- Colleges, Schools and Child Care Providers
- Long-term Care Facilities
- Travelers
Information that could help everyone includes:
- What is COVID-19?
- Frequently Asked Questions
- Latest Updates for NC: COVID-19 case count, weekly updates, list of websites and social media to find reliable COVID-19 information.
- News Releases
- Stigma: What can be done to combat fear and anxiety.
- Community Events: Guidance for community events and mass gatherings.
- Materials and Resources: Materials available for use on social media or for downloading and printing.
AMA Creates CPT Code for COVID-19
For quick reference, the new Category I CPT code and long descriptor are:
- 87635 Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique
The code is effective immediately for use as the industry standard for reporting of tests for the novel coronavirus across the nation’s health care system. In addition to the long descriptor, CPT code 87635 has short and medium descriptors that can be accessed on the AMA website.
Last Week's Provider Forum Answers Frequently Asked Questions
Last Friday’s Forum Answered Some of Your Pressing Questions
Last Friday, NC DHHS and NC AHEC offered its first call-in Forum for health care professionals to answer questions you have about response to Covid-19. Below are some of the broad categories of questions with links to the latest information posted on the NCDHHS and CDC webpages.
Another call-in Forum is slated for this Friday, March 20 from 12:30 to 1:30 p.m. Please submit your questions by 5 p.m. on Wednesday to [email protected].
Access the forum through your computer at https://zoom.us/j/705979628. Or you can dial-in for audio-only, by calling 1-646-558-8656 and entering the conference ID: 705979628#.
During last Friday’s Forum, NCDHHS Medical Epidemiologist Erica Wilson, MD, MPH, answered questions and offered resource links in the following areas:
Who to test for Covid-19:
While we’re in cold and flu season, Dr. Wilson stressed it is important to distinguish the broad range of Covid-19 symptoms from a cold or flu. At this point, a person who is asymptomatic, should not be tested, she said.
As of Friday, the state lab and LabCorp were performing tests for Covid-19. For testing through the state lab, prior approval by your local health department or the state epidemiologist on call is necessary. Testing through LabCorp does not require prior approval.
Symptom criteria for testing:
- Fever OR signs/symptoms of lower respiratory illness (e.g., cough, shortness of breath) in any person, including healthcare workers, who has had close contact with a laboratory-confirmed COVID-19 patient within 14 days of symptom onset.
- Fever AND signs/symptoms of lower respiratory illness (e.g., cough, shortness of breath) AND negative influenza test (rapid or PCR) and no other more likely diagnosis.
Here is the latest NCDHHS guidance on testing, specimen collection and shipping.
Here is LabCorp’s guidance document.
Dr. Wilson said that NCDHHS is working to compile a comprehensive list of clinics, public health departments and hospitals throughout the state that are equipped to offer testing.
She also said that as of Friday afternoon, the turnaround time for test results from LabCorp was three to four days. The state lab turnaround time depends on volume of test orders.
Once a person has been tested, Person Under Investigation (PUI) protocols are initiated, in which the person is isolated pending the test results. Learn more about these protocols.
Dr. Wilson also stressed that this is a reportable condition.
Personal Protective Equipment
Dr. Wilson directed health care providers to the Centers for Disease Control and Prevention (CDC) website for the latest on personal protective equipment (PPE) requirements. Someone is at risk of infection if they are within six feet of a person who is infected with the virus for at least 10 minutes and/or come in contact with any respiratory secretions from that person.
She urged clinics that do not have adequate PPE to find another location in the community where people may be seen or tested. NCDHHS is currently compiling a list of facilities in each county that can accommodate patients being sent to them. Ultimately, the individual practice will have to make the decision on seeing patients who may need to be tested, she said.
If you have questions about PPE, she encouraged you to send them to [email protected]
Other information from the Forum
In answer to other questions during the Forum, Dr. Wilson said that the specifics for Covid-19 as far as viral shedding and spread are still not known.
When asked if the warmer spring and summer weather would perhaps mitigate the spread of the virus, she only commented: “We’ll see.”
Wake County Health Department Offers COVID-19 Help
The Wake County Health Department has compiled a list of Q&As to assist in getting the information health care professionals need about this evolving situation, while also providing a better understanding of public health’s role in working to contain this novel coronavirus. Access that list.
Some of the questions addressed in the FAQs include:
• What should I do with a patient who is exhibiting the symptoms associated with COVID-19?
• Who should be tested for COVID-19?
• What if one of my patients test positive for COVID-19?
• How can our office test for COVID-19?
• What is my risk to my staff and providers?
• Should I send patients that need COVID-19 testing to the Wake County Health Department for testing?
You can visit the Wake County Health Department’s COVID-19 webpage, which has a set of frequently asked questions to educate providers. You can also email the department questions at [email protected], or you can call its COVID-19 information line at 919-856-7044. The county is also sharing important information on its Facebook, Twitter and Instagram accounts.
NC Medical Board Adopts Emergency Rules in Response to COVID-19
The NC Medical Board (NCMB) and the NC Rules Review Commission have approved emergency rules allowing a physician or PA who inactivated his or her NC medical license within the past 24 months to quickly obtain a temporary license to support Gov. Roy Cooper’s declaration of a state of emergency due to Covid-19. The license would authorize the physician or PA to practice for 90 days or until the state of emergency in North Carolina is declared over. Read the rules.
Over the next few days, NCMB will develop an online application form to receive temporary license requests from interested physicians and PAs. We expect to have this application ready by sometime next week. NCMB is not currently accepting requests for the new temporary emergency license.
Issuance of temporary authority to practice is subject to the following conditions:
- The applicant must demonstrate that he or she has practiced clinical medicine for at least 80 hours during the most recent 24 months;
- The applicant must have been licensed continuously for at least 10 years prior to making his or her medical license inactive;
- The applicant must have no history of public discipline and must not have inactivated his or her license while under investigation; and
- The applicant must confine his or her practice to areas in which he or she is clinically competent.
Please note that the NCMB adopted the emergency rules to support the Governor’s declaration of a state of emergency, which identifies a need to develop additional medical resources in the state, including additional providers. This is a preparedness step – there’s no indication that there’s a current need for additional medical providers to assist with COVID-19.
NCMB will likely advise inactive physicians and PAs who may be interested in returning to practice to check in with their local public health departments, former employer/practice, local hospital or other health care employer to determine if they are needed.
For the most up-to-date information visit the NCMB website.
Political Pulse for March 6, 2020: Election Results
Chip Baggett is back with Sue Ann Forrest to provide a quick summary of primary election results for physicians and PAs running in the state. Check out the video below and be sure to offer your input on this weekend's Sunday Survey on insurance payer improvements. Many thanks to those who responded to last week's survey; if you missed the recap of results in Morning Rounds, you can view those here.
NCMS Political Pulse for Feb. 21, 2020
NCMS Director of Legislative Relations Sue Ann Forrest, MPA, shares information on her recent advocacy talks and also reminds viewers that early voting ends Feb. 29. In addition, she asks that NCMS members keep an eye out in March for advocacy surveys where they can share their feedback on priority legislative issues.
Winter Edition of the NCMS Bulletin Now Available
 The latest issue of the online NCMS Bulletin Magazine is now available. This edition focuses on physician wellness, offering expert insights, stories from your colleagues and practical tips to help create a practice environment that promotes wellness.
The latest issue of the online NCMS Bulletin Magazine is now available. This edition focuses on physician wellness, offering expert insights, stories from your colleagues and practical tips to help create a practice environment that promotes wellness.
Articles include:
- "The 'Veep of Joy' and the Practice Transformation Initiative" featuring Christine Sinsky, MD;
- "WEPPA & Wellness: A Successful Balancing Act" featuring Wake Emergency Physicians' Nancy Adams and Paul Bobryshev, MD;
- "Workplace Health: How to Practice Wellness" featuring Curi's Jason Horay and health coach Rachel Druckenmiller;
- "Releasing the Pressure: One Physician’s Journey to Well-Being" featuring Naomi "Betsy" Simon, MD;
- "How a Scribe Changed a Physician’s Life" featuring Michelle Jones, MD;
- "NC Medical Board Moves to Support Physician Well-Being" featuring Damian McHugh, MD, FACEP.
Political Pulse for November 22, 2019
Get the scoop on what the delay in Medicaid Transformation means for you from Chip Baggett and Sue Ann Forrest in this week's Political Pulse.
MEDTalks 2019: Lynn Bowlby, MD -- "Palliative Care Training for All"
Lynn Bowlby, MD, an internal medicine physician in Durham, shares her thoughts on why palliative care training is so important for all physicians in her MEDTalk.
MEDTalks 2019: Derek Clar -- "Anesthesia, Pain and Fewer Opioids"
Derek Clar, a Campbell University School of Osteopathic Medicine student, offers the results of "Post-Operative Opioid Use and Practices: Developing a Physician Intervention to Decrease Excessive Opioid Prescribing in Cesarean Sections for the Management of Postoperative pain."
MEDTalks 2019: Sue Ann Forrest, MPA -- "Health Policy & Physician Engagement"
NCMS Assistant Director of Legislative Relations, Sue Ann Forrest, MPA, shares her findings in her MEDTalk: "Where are Physicians in Advocacy? Participation Counts and Showing up Matters."
MEDTalks 2019: Garett Franklin, MD -- "Student Athlete Web-Based Concussion Tool"
Dr. Garett Franklin, a family medicine physician in Cary, details his Leadership College project "BONK!
Keeping Student-Athletes Safe in the Field of Play," a telemedicine tool for student athletes and their families, trainers, coaches, physicians and others to track and measure potential head trauma.
MEDTalks 2019: Quinnette Jones, PA-C -- "Physician Assistant Leadership"
Quinnette (Quincy) Jones, MSW, MHS, PA-C, a PA in Durham, shares her findings on "Physician Assistants and Leadership:
Training, Experiences and Needs in NC."
MEDTalks 2019: Satish Mathan, MD -- Transportation as a Social Determinant for Radiological Exams
Dr. Satish Mathan, an interventional and vascular radiologist in Raleigh, examines the "Impact of Transportation Social Determinant on Patient Access to Lower Cost Outpatient Imaging."
MEDTalks 2019: David E. Melon, MD -- "Leveraging Employee Engagement to Drive Patient Experience"
Dr. David Melon, an otolaryngologist from Hickory, shares his MEDTalk that focuses on engaging practice employees to improve patient experience.
MEDTalks 2019: Gaurang Palikh, MD, FAAN -- "Teleneurology"
Dr. Gaurang Palikh, a neurologist from Shelby, explores "The Case for Teleneurology to Address Critical Shortages in North Carolina and Beyond: Using Technology to Solve Old World Problems" in his MEDTalk.
MEDTalks 2019: Edward Ricciardelli, MD -- "Patient Positioning for Pressure Ulcers"
Dr. Edward Ricciardelli, a plastic surgeon in Wilmington, shares his MEDTalk on the "Effect of The LEAF Patient Monitoring System on Turning Compliance in the ICU Setting."
MEDTalks 2019: Vinay Saranga, MD -- "Smoking Cessation Training"
Dr. Vinay Saranga, a psychiatrist in Apex, shares the results of his Leadership College project on "Easter Seals Tobacco Treatment Training," which takes the mental health needs of patients into consideration.
MEDTalks 2019: Evan Simmons -- "Assessing and Facilitating Board Needs"
Evan Simmons, NCMS Director of Executive and Board Services, shares her MEDTalk "Identifying Opportunities of Engagement and Development by Discovering Gaps in Perception of Board Roles and Responsibilities."
MEDTalks 2019: Lindsay Strowd, MD -- "Teledermatology"
Dr. Strowd, a dermatologist from Winston-Salem, shares her talk on "Utilizing EMR-Based Technology to Improve Access to Dermatology."