Register Now! AMA Advocacy Insights Webinar: Strategies to Address the Nation’s Worsening Drug Overdose and Death Epidemic

Registration is open for the next webinar in the AMA Advocacy Insights series – “Strategies to address the nation’s worsening drug overdose and death epidemic” – on December 12 at 11:30 a.m. Central time.
The 2023 AMA Overdose Epidemic Report finds that – despite positive actions from physicians, growth in harm reduction services, and policy advancements – the nation’s drug overdose and death epidemic is deadlier than ever. The annual report details many of the reasons the epidemic persists, largely due to illicitly manufactured fentanyl and the continued lack of meaningful implementation and enforcement of policies that support affordable, accessible, and evidence-based care for patients with substance use disorders or pain.
Learn more in this webinar about policy actions that need to be taken, harm reduction strategies that should be implemented more broadly, and efforts by physicians and the AMA Substance Use and Pain Care Task Force to end the epidemic.
EXTENDED! More Time to Meet Making Care Primary Application Deadline
DEADLINE EXTENDED!

The Centers for Medicare & Medicaid Services (CMS) has announced a new voluntary value-based primary care model called Making Care Primary (MCP). With a planned launch date of July 1, 2024 in eight states, including North Carolina.
The 10.5-year model aims to improve care management and care coordination, equip primary care clinicians with tools to form partnerships with health care specialists, and leverage community-based connections to address patients’ health needs.
CMS is now accepting non-binding applications from Medicare-enrolled organizations that provide primary care services to fee-for-service Medicare beneficiaries. The application deadline is December 14, 2023.
NC AHEC has developed an MCP playbook for potential applicants, which contains concepts about the MCP model and its design, timelines, evaluation tools, considerations, and resources. It's a must-see for those interested in applying!
For more information, visit CMS here.
Medicaid Expansion Could Help North Carolina's Overdose Crisis
NCDHHS says that between 2000 and 2022, more than 36,000 North Carolinians lost their lives to drug overdose.

There could be some relief coming to rural areas in North Carolina that continue to deal with the opioid crisis. Better treatment options are some of the benefits of Medicaid expansion, according to Kody Kinsley, the secretary of the state’s Department of Health and Human Services.
Kinsley described overdose losses as “deaths of despair” — saying they often occur when people are struggling with mental illness, lack social connection or have a negative life event such as a job loss.
He says many people who could not get treatment in the past will now be able to do so through the Medicaid expansion that began last week. He says with the right care and support, they can reconnect with those around them.
“They're working again, they're taking care of their families, they're paying taxes, they're supporting their rural communities and they're making it vibrant,” he says.
Kinsley says there’s another benefit to getting rural residents with drug addictions medical help under Medicaid: it will take a burden off local law enforcement. [source]
20 NC Hospitals Receive High Honors for Maternity Care

More than 20 North Carolina hospitals were rated among the best regional hospitals for maternity care, according to U.S. News and World Report.
On Tuesday, the publication released its list of the best hospitals for maternity care for uncomplicated pregnancies.
UNC Hospitals in Chapel Hill, UNC Rex Hospital in Raleigh, WakeMed Hospital in Cary and Raleigh and Duke Regional Hospital in Durham were all named high-performing in maternity care.
North Carolina hospitals that were named high-performing for maternity care for uncomplicated pregnancies:
- Alamance Regional Medical Center
- Atrium Health-Cabarrus
- Atrium Health-Pineville
- Atrium Health-University City
- Catawba Valley Medical Center
- Duke Regional Hospital
- Moses H. Cone Memorial Hospital
- Novant Health Forsyth Medical Center
- Novant Health Huntersville Medical Center
- Novant Health Matthews Medical Center
- Novant Health New Hanover Regional Medical Center
- Novant Health Presbyterian Medical Center
- Novant Health Thomasville Medical Center
- UNC Hospitals
- UNC Rex Hospital
- WakeMed Cary Hospital
- WakeMed Raleigh Campus
“Hospitals that receive a High Performing designation as part of Best Hospitals for Maternity Care meet a high standard in caring for parents with uncomplicated pregnancies,” said Jennifer Winston, Ph.D., health data scientist at U.S. News. “These hospitals have C-section rates that are 26% lower, and newborn complication rates that are 37% lower than unrecognized hospitals that participated in the survey. Parents-to-be can research their local hospitals’ performance metrics for free at health.usnews.com to help them choose where to have their baby.” [source]
Join DOCMS' Final Meeting of the Year
Join DOCMS at the University Club!
Wednesday, December 13, 2023 | 6:00pm - 8:00pm
University Club, 3100 Tower Boulevard, Suite 1700 - Durham, NC 27707
AGENDA:
- 6:00pm- 6:30pm – Socializing & Housekeeping
- 6:30pm- 7:30pm – Dinner & Guest Speaker
- 7:30pm- 7:45pm – Q&A
- 7:45pm- 8:00pm – DOCMS 2023 Business
REGISTER NOW - Hybrid Meeting
"Burnout; why is the intensity of the flame worsening, despite increasing research and awareness?"
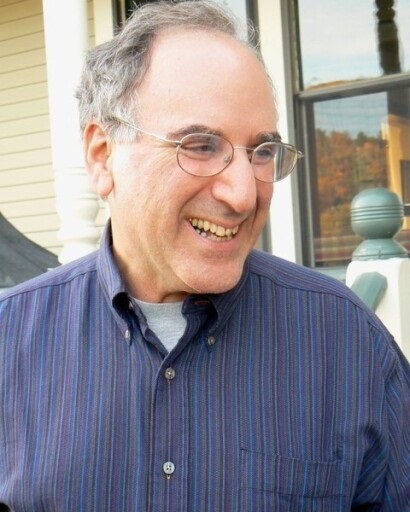
Dr. Damian McHugh

A two-way discussion about “why is the data-do gap getting worse”. We have known about burnout for 40+ years, so why is it now critical in medicine – and law, in our military, animal vets and teachers?
This article will be a nice compliment to the discussion.
Dr. Damian McHugh bio:
Proud father of two hungry teens, eager (but still poor) golfer, husband of Marion – trauma nurse turned travel nurse consultant, I graduated Med School in 1990 at Manchester UK. Having become a member of the Royal College of GPs, I swerved specialties and changed countries. Having repeated a full EM Residency at UNC, I spent 21 wonderful years at the Rex ER in Raleigh.
Since ending my clinical practice, I've been afforded the privilege of walking the back 9 of my career as SVP Physician Liaison at Curi, a full-service physician advisory firm headquartered in Raleigh. Each day that I wake, I'm driven to discover how better our company (which is owned by its 14,000+ member physicians) can make their lives better in Medicine, Business and Life.
I'm passionate about burnout, having seen so many colleagues brought to their knees by a complex medical system that so often appears to place dollars ahead of patients and their providers.
REGISTER NOW - Hybrid Meeting
Questions or can you not open the registration google link?
Please email Frank Snyder at [email protected]
1 CME Credit is available! Click here for how to claim your credit.
DOCMS Members & Prospective Members - FREE to attend
Guests - $25 to attend (will be collected at meeting site)
A Zoom link will be sent to registered attendees on August 9th.
NCTracks December Provider Training Schedule Now Available

Registration is open for the December 2023 instructor-led provider training courses. NCTracks Zoom courses can be attended remotely from any location with a computer and internet connection. Individualized meeting information has been created for each course.
Courses include:
- Submitting a Professional Claim- Provider NEMT
- New Office Administrator
- Recipient Eligibility Verification
- Prior Approval Medical
- Submitting Professional Claims
- Dental Helpful Hints
Please see the Course Information and Training Enrollment Instruction details here.
NCMS Leadership College Alum Named President of NCAFP
NCMS member and Leadership College Alum Dr. Garett Franklin named President of the North Carolina Academy of Family Physicians.

Dr. Garrett Franklin, a native of Drexel, NC, is the new president of the North Carolina Academy of Family Physicians. He attended North Carolina State University graduating with a BS in engineering in 2003, a BA in chemistry in 2007 and a Masters of Physiology in 2008. He completed medical school at the Brody School of Medicine at East Carolina University in 2012 and went on to complete his family medicine residency and a primary care sports medicine fellowship at Wake Forest Baptist Medical Center.
Franklin became involved in the NCAFP’s advocacy efforts as a resident at Wake Forest and has served on the Board of Directors for the last five years. He practices family medicine and sports medicine at Raleigh Medical Group/Cary Medical Group in Raleigh, while also working at NC State University as a team physician. He is active in academic and clinical research and many advocacy projects.
Franklin and his wife have a son and daughter and live in Raleigh. He has been a member of the North Carolina Medical Society since 2008.
NC DHHS Launches New Performance Dashboard for 988 Suicide and Crisis Lifeline

The North Carolina Department of Health and Human Services has launched a performance dashboard for the 988 Suicide and Crisis Lifeline to highlight how the suicide and crisis lifeline is being used in North Carolina.
The 988 Suicide and Crisis Lifeline connects North Carolinas via call, chat or text to a trained crisis counselor who will listen, offer support and provide community resources 24 hours a day, 7 days a week. 988 is a state-federal partnership between NCDHHS and the U.S. Substance Abuse and Mental Health Service Administration. It was implemented nationwide in July of 2022.
"North Carolina is a national leader in operationalizing 988 which is a critical part of the state's crisis system," said NC Health and Human Services Secretary Kody H. Kinsley. "With shortened response times and more connections made, 988 is a powerful tool in helping to get North Carolinians the support and resources they need when they need them."
The dashboard shows North Carolina is successfully meeting demand for the 988 service. North Carolina outperforms national averages in several key areas. For example, it takes 14 seconds to answer calls in North Carolina whereas the national average is 39 seconds. North Carolina also answers 98% of all calls received, compared to the national average of 90%. And the dashboard indicates a 25% increase in utilization over the past year, which shows the service is playing a valuable role for North Carolinians in need of mental health resources.
The 988 performance dashboard provides useful information on contact volume, answer rates, speed of answer, age ranges and reasons for calling. It also indicates call volume for specific populations, including North Carolinians who reach out to the Spanish call center, Veterans Crisis Line and the LGBTQ+ youth and young adult line (e.g., the Trevor Project Line). Data shared in the dashboard does not include personal or confidential health information.
"Understanding how this service is being used and by whom are keys to understanding where our crisis system is working well and where it needs to be improved," said Kelly Crosbie, MSW, LCSW, Director of the NCDHHS Division of Mental Health, Developmental Disabilities, and Substance Use Services. "The 988 dashboard will help us build the accountability necessary to ensure people get care they need when and where they need it."
988 is an important component of our overall crisis system. The new state budget invests $131 million to expand and strengthen crisis services in North Carolina. In addition to 988, several key community-based crisis services are funded, such as:
- Mobile Crisis Teams: Immediate, on-site support for people experiencing a mental health and/or substance use crisis
- Facility-Based Crisis Centers and Drop-in Centers: Community-based crisis centers for individuals experiencing a behavioral health or substance use crisis
- Non-Law Enforcement Pilot Program: Transportation services to psychiatric facilities that do not involve law enforcement
- Behavioral Health (BH) SCAN: Statewide bed registry that helps hospitals and other providers facilitate and track referrals and access to inpatient, crisis, residential and community levels of care
The department is currently developing its implementation plan for these investments and is keeping people informed through a monthly webinar titled "Side By Side." It is hosted by the Division of Mental Health, Developmental Disabilities, and Substance Use Services. For more information, or to register as an attendee for one of these webinars, please visit the Side By Side meeting registration link.
988 is available to anyone, anytime. If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org. Individuals who speak Spanish can now connect directly to Spanish-speaking crisis counselors by calling 988 and pressing option 2, texting "AYUDA" to 988, or chatting online at 988lineadevida.org or 988Lifeline.org.
Prescription Reimbursement Change for Non-Medicaid Enrolled Providers

Medicaid expansion launched on December 1, 2023, and NC Medicaid is reminding providers that prescriptions written by non-Medicaid enrolled providers will not be reimbursable by NC Medicaid due to federal requirements. NC Medicaid requires that all providers whose NPI will be used on a pharmacy claim be enrolled with NC Medicaid. There are no exceptions to this requirement. This bulletin applies to NC Medicaid Direct and NC Managed Care.
NC Medicaid anticipates close to 300,000 new beneficiaries will receive full Medicaid coverage through Medicaid expansion on Dec. 1, 2023. Many of these beneficiaries may have had primary care services in free and charitable clinics who do not bill and are not enrolled in NC Medicaid.
- This means that beneficiaries with prescriptions from non-Medicaid enrolled individual providers will be denied coverage, and the beneficiary will not be able to fill their prescription through the NC Medicaid benefit.
- The pharmacy may fill the prescription at full cost for the beneficiary.
For clinics that dispense medications at no cost to patients, providers should consider dispensing an additional 30-day supply of medications to support the new Medicaid beneficiary during the transition period to allow time for beneficiaries to engage with their new NC Medicaid provider and/or time for non-Medicaid providers to enroll in NC Medicaid. Non-enrolled providers are encouraged to consider enrolling in NC Medicaid so prescriptions can be covered benefits.
To receive payment for office visits for Medicaid beneficiaries, a provider must fully enroll; however, there is a “lite” enrollment option that will allow providers to enroll as an Ordering, Prescribing, Referring (OPR) provider.
- The OPR provider enrollment process is a simpler and easier path to enroll into NC Medicaid only for the purposes of ordering, prescribing and/or referring beneficiaries for services.
- The estimated completion time for OPR provider enrollment is approximately one to two weeks from the application submission (if there are no issues with the submitted application).
- Enrolling as an OPR only provider would enable providers to prescribe medications, which are billed to NC Medicaid by the pharmacy, without the provider having to enroll as a full rendering Medicaid provider.
- If a provider would like to continue to serve NC Medicaid beneficiaries, providers must enroll as a full Medicaid provider.
Non-Medicaid enrolled providers treating beneficiaries who will enroll in NC Medicaid through Medicaid expansion should submit an OPR application as soon as possible. To enroll in NC Medicaid as an OPR only provider, providers can go to the NCTracks Provider Enrollment page.
- Under Quick Links, there is a user guide for “How to Enroll in NC Medicaid as an Individual Practitioner.”
- Select “Ordering, Prescribing, Referring Providers Enrolled with the Lite Application” (or if fully enrolling, select “Individual Full Enrollment”) as the Provider Enrollment Application Type.
- After submitting the application, applying providers should make sure to quickly respond to any notification regarding the application and reach out for assistance as soon as needed to ensure quick resolution of any open items impacting enrollment.
For more information on OPR provider enrollment, please review the OPR Provider FAQs.
When pharmacies process prescriptions for NC Medicaid beneficiaries that are denied due to the provider not being enrolled, pharmacists should encourage beneficiaries to schedule an appointment with their new NC Medicaid enrolled provider as soon as possible.
Beneficiaries should also be encouraged to seek out urgent care, Federally Qualified Health Centers (FQHCs) or the emergency department if they have an immediate need for medications to avoid gaps in care. Additionally, if the beneficiary received a prescription from a free clinic, the beneficiary should be encouraged to go back to the free clinic to refill their prescription until they are able to set-up an appointment with their NC Medicaid provider. Pharmacists are also encouraged to reach out to non-Medicaid enrolled providers regarding enrollment and to inquire if there is another NC Medicaid provider with an established relationship with the beneficiary who can write a new prescription for the beneficiary.
In summary, please see the below actions for prescribers and pharmacies:
1. Actions for Prescribers: Non-Medicaid enrolled providers treating a beneficiary enrolling in NC Medicaid through Medicaid expansion should consider applying to enroll in NC Medicaid. No additional action is needed for actively participating providers.
- To receive payment for office visits for Medicaid beneficiaries, a provider must fully enroll in NC Medicaid.
- If the only intent is to ensure prescriptions are paid by Medicaid, non-enrolled providers may choose the lite enrollment option which only allows claim payment when the provider is ordering or referring for services or prescribing medications. The lite provider enrollment process is a simpler and quicker way to enroll into NC Medicaid when the provider does not intend to bill for rendered services.
2. Actions for Pharmacies: When pharmacies process prescriptions for NC Medicaid beneficiaries, which deny due to the provider not being enrolled, they should:
- Contact non-Medicaid enrolled providers regarding enrollment and to inquire if there is another NC Medicaid provider with an established relationship with the beneficiary who can write a new prescription for the beneficiary.
- Encourage beneficiaries to schedule an appointment with their new NC Medicaid enrolled provider as soon as possible.
- Encourage beneficiaries to seek out urgent care or the emergency department if they have an immediate need for medications or a medical emergency.
- Encourage beneficiaries to go back to the free clinic (if applicable) to refill their prescription until they are able to set-up an appointment with their NC Medicaid provider.
For questions, contact NCTracks Call Center: 800-688-6696
Register Now for Improving Child and Youth Mental Health Webinar Happening Tomorrow

The Improving Child and Youth Mental Health: Driving Factors and Root Causes webinar will highlight the report, Addressing the Long-Term Effects of the COVID-19 Pandemic on Children and Families (2023).
Drawing on the work of the Board on Children, Youth, and Families in the Division of Behavioral and Social Sciences and Education and the Health and Medicine Division at the National Academies of Science, Engineering, and Medicine, this webinar will focus on the driving factors that contribute to the children and youth mental health crisis, including disparities and inequities in the mental health system.
Speakers will include:
- Leslie Walker-Harding, Division Chief and Director Ford/Morgan Endowed Professor and Chair, Seattle Children's Hospital (Moderator)
- Margarita Alegria, Professor, Departments of Medicine & Psychiatry, Harvard Medical School, Chief, Disparities Research Unit, Department of Medicine, Massachusetts General Hospital, Harry G. Lehnert, Jr. and Lucille F. Cyr Endowed Chair, Mass General Research Institute, Massachusetts General Hospital
- Tumaini Rucker Coker, Professor and Division Head of General Pediatrics, University of Washington School of Medicine, and Seattle Children’s Hospital
- Kimberly E. Hoagwood, Cathy and Stephen Graham Professor of Child and Adolescent Psychiatry, New York University Langone Health
- Caren Howard, Senior Director, Policy and Advocacy, Mental Health America
Happy Birthday to These NCMS Members Celebrating This Month!
Grab your party hats and noisemakers and let’s celebrate!
Randy S. Adams, MD
Swati S. Adawadkar, MD
Briggs M. Ahearn, MD
Collette Ah-Tye, MD
Edward S. Alessandrini, DMD, MD
Richard J. Alioto, MD
E. Jackson Allison, Jr., MD, MPH
Simon J. Allport, MD
Barry D. Amos, MD
Swathi B. Anche, MD
Sarah M. Anderson, MD
Wallace F. Andrew, Jr., MD
Bradley L. Anglemyer, MD
William E. Anthony, Jr., MD
Andrew P. Apicella, PA-C
Gregory C. Appert, MD
Ana M. Arango, MD
Perico N. C. Arcedo, III, DO
Dina L. Arceo, MD
Louis C. Argenta, MD
Tracy O. Arusuraire, MD
Nancy J. Astle, MD
Savana E. Atkins, PA
Sam T. Auringer, MD
T. James Baden, MD, FACP
Charles E. Baker, MD
Vansanth B. Baliga, MD
Charles L. Baltimore, Jr., MD
W. Byron Barber, II, MD
Joseph U. Barker, MD
Christopher J. Barnes, MD
Laura A. Barton, PA-C
Laura B. Barton, PA-C
Karen L. Bash, MD
Tara K. Bastek, MD
Sanjay Batish, MD
Gregory S. Bauer, MD
Margaret R. Beal, PA-C, MMS
V. Edward Bean, MD
L. Neal Beard, Jr., MD
Walter B. Beaver, Jr., MD
Gregory G. Bebb, MD
Michelle L. Beckham, MD
Timothy M. Beittel, MD
James E. Bellard, MD
Barbara A. Bergdolt, MD
Donald R. Bergsma, Jr., MD
Chudaratna Bhargava, MD
Edgardo H. Bianchi, MD
Karl F. Bitter, MD
James F. Black, MD
Jesse A. Blackman, MD
Susan Blackwell-Crawford, PA-C
Benjamin R. Blaschke, PA-C
Seth J. Bleier, MD
Charles J. Blevins, MD
Robert J. Board, MD
Edwyn T. Bowen, Jr., MD
James H. Bradford, MD
Genevieve N. Brauning, MD
Karen E. Breach Washington, MD
Katherine L. Breiter, MD
Samuel E. Britt, II, MD
M. Todd Brown, MD
Natalie Bruce, MD
George F. Brumback, MD
Tracie C. Bryson, MD
Joseph A. Buglisi, Jr., DO
Kerry C. Bullerdick, MD
Nicole P. Bullock, MD
Richard A. Bunio, MD
Holly J. Burge, MD
Rollin S. Burhans, Jr., MD
J. P. Burnette, MD, FACP
Brandon C. Burnsed, MD
D. Scott Burton, MD
Jeffrey W. Byrnett, MD
Marco A. Caceres, MD, FACS
T. Francis Camp, Jr., MD
Leah A. Carlson, MD
Kevin W. Carroll, MD
Fred A. Caruso, MD
Venkata R. Challa, MD
H. Royster Chamblee, Jr., MD
Jeffery A. Chance, PA-C
E. Ted Chandler, MD
Ku-Lang Chang, MD
Benjamin C. Chasnis, DO
Abdul G. Chaudhry, MD, FACS
Nicole R. Check, MD
Peter G. Chikes, MD, FACS
Terry C. Childers, MD, FAAP
Stephanie M. Chismar, DO
Stephen K. Chiu, MD
San H. Choi, MD
Windy D. Christy, PA-C
Derek Clar, DO
Erika L. Clark-Trapp, MD
Shelby L. Clay-Rogers, MD
Richard B. Clinton, MD
Bruce E. Cohen, MD
James B. Collawn, MD
Filiberto Colon, II, MD
Jessica S. Connett, MD
Tim E. Cooper, Jr., MD
Charles I. Cooperberg, MD
Anureet C. Copeland, MD
A. James Coppridge, MD
Asa L. Cordle, MD
Joseph B. Cornett, MD
Benjamin B. Covell, MD
Chad E. Cox, MD
Karen L. Cross, MD
James J. Crossley, MD
John T. Curnes, MD
John W. Currens, MD
Mark A. Curzan, MD
Samuel J. Dail, MD
Liam N. Daly, MD
Aaron P. Danison, DO
Uma U. Darji, MD
Marc A. Darst, MD
David A. Dasher, MD
Andrew Davidson, MD
Kevin R. Davidson, MD
D. Whitaker Davis, MD
Devon L. Davis, MD
Robin L. Dawson, PA-C
Ernesto E. de la Torre, MD
Patricia Y. De Tomas-Medina, PA-C
James P. Deering, III, MD
John O. delCharco, MD
Jessica C. Derreberry, MD
Christopher F. Dibble, MD
Edward E. Dickerson, IV, MD
Ellen D. Dillavou, MD
Michael J. Donahue, MD, FAAD
Venkatarama S. Donepudi, MD
Kristin L. Donoghue, MD
Kevin E. Dougherty, MD
Ryan C. Dougherty, MD
Caron L. Dover, MD
Carrie A. Dow-Smith, MD
Laurel L. Drayton, PA-C
Melora T. Driver, MD
Vincent J. D'Souza, MD
Frederick M. Dula, Jr., MD
Raymond B. Dyer, MD
Matthew D. Dyson, MD
J. William Eakins, MD
R. Crews Edens, PA-C
Kim D. Edhegard, II, MD
Lorven M. Edralin, MD
Amanda E. Edwards, PA-C
Charles D. Edwards, MD
Stephen P. Ellison, MD
Miles Elmore, MD
John A. Engelmann, Jr., MD
Nathaniel Erskine, MD
Joseph J. Estwanik, MD
Anna F. Fakadej, MD
Ann E. Farash, MD
Bruce E. Fee, MD
Dale E. Feldpausch, Jr., MD
Ana C. G. Felix, MD
Juan B. Firnhaber, MD
David M. Fisher, MD
Lara L. Fisher, MD
Kellie E. Flock, PA-C
Rajat R. Fofaria, MD, FACC
Richard S. Foulke, MD
James J. Foutty, MD
Casey N. Fox-Morea, PA-C
Nicholas Frankel, MD
Mel W. Fryar, MD
Kiana M. Fussner, PA
Walter H. Gajewski, MD
P. Mark Gallerani, MD
Gabryel L. Garcia-Sampson, MD
Lars B. Gardner, DO
W. Ronald Gardner, MD
Edgar C. Garrabrant, III, MD
James E. Garrett, MD, FACEP
Joshua E. Garriga, MD
Scott K. Garrison, MD
Cynthia M. Gary, PA-C, MPH
Byron M. Geer, DO
Ashley L. Gelinas, MD
Henry Gerock, MD
Martin T. Gessner, MD
Robert W. Gibson, MD
Charles D. Godwin, MD
Geraldine F. Goertzen, MD
Manuel J. Gorrin-Rivas, MD, PhD
James A. Graham, MD
James J. Green, Jr., MD
P. David Green, MD
Kimberly M. Greenwald, MD
Kathryn M. Greven, MD, FASTRO
Andrew S. Griffin, II, MD
Joe W. Grisham, MD
Christopher T. Grubb, MD
Cesar Guajardo, MD
W. Bonner Guilford, MD
Ashraf F. Guirgues, MD
Jagmohan D. Gupta, MD
Khie S. Ha, MD
Michel G. Haddad, MD
M. Suzanne Hampson, MD
Aaisha S. Haque, MD
Kyle C. Harner, MD
Charles D. Harr, MD
Phillip G. Harris, MD
Samuel R. Harris, MD
Joseph S. Healy, MD
Jessica A. Hedrick, PA-C
Scott A. Hees, DO
Steven M. Heffner, MD
Craig S. Heinly, MD
William R. Henrick, MD
Richard C. Herring, MD, MBA
Heath C. High, MD
Philip L. Hillsman, MD
Kiem M. Hioe, MD
Angela S. Hira, DO
Jonathan N. Ho, MD
Mary K. Hoffman, MD
Carla W. Holder, MD
Christopher M. Holland, MD
Michael D. Holland, MD
Walter B. Holland, MD
Steven D. Hollosi, DO
John D. Holly, MD
Kenneth A. Holt, MD
W. Borden Hooks, III, MD, FACS
Jennifer J. Hoover, MD
Teague L. Horton, MD
Frank M. Houston, MD
Joshua L. Hudgens, MD
Alese V. Hunt, MD
James A. Hunter, MD
Joseph T. Inglefield, III, MD
Thomas G. Irons, MD
Hicham S. Ismail, MD
Mark T. Jackson, MD, FAAP
Ashok Jain, MD, MBA, FAAP
Francis M. James, III, MD
Edward O. Janosko, II, MD, FACS
Jennifer A. Jarosz, MD
S. Taylor Jarrell, MD
Robert G. Jeffers, MD, MPH, FAAP
Robert B. Jennings, MD
Rupert W. Jilcott, III, MD
Suresh Jillellamudi, MD
Carrie E. Johnson, MD
Delores L. Johnson, MD, FACOG
Matrika D. Johnson, MD
Ryan C. Johnson, MD
John D. Johnston, MD
William O. Jolly, III, MD
Enrico G. Jones, MD
James D. Jones, MD
Jason D. Jones, MD
J. W. Jones, MD, FACP, AGAF
Allen M. Joseph, MD
Ismo M. Kaariainen, MD
Jacob A. Kahn, MD
Scott M. Kahn, MD
Haku K. Kahoano, MD
David M. Kaplan, MD
Christina M. Karr, PA-C
Sanjeev Katyal, MD
Douglas G. Kelling, Jr., MD, FACP
Jeffrey S. Kelly, MD
William H. Kelly, MD
Kirsten S. Kerr, MD
Christine M. Khandelwal, DO
Gautam Khandelwal, MD
Khalid W. Khayr, MD
George R. Kilpatrick, Jr., MD
Whitney L. Kirchoff, MD
Richard E. Kleinmann, MD
J. Douglas Knoop, MD
Lawrence H. Knott, Jr., MD, FACS
William G. Kodzai, Jr., MD
Sarath C. Kolluru, MD
Shawn D. Kosnik, DO
Paul J. Kostuchenko, MD, PhD
William H. Kouri, MD
Kevin L. Krasinski, MD
Jack J. Kuritzky, MD
Cameron J. Kurowski, MD
Ryan P. Lamb, MD
Graham G. Lashley, MD
Mark K. LaVigne, MD
Marley B. Lawrence, MD
David L. Leader, Jr., DO
Tami A. Lee, PA-C
William D. Lee, Jr., MD
Gail A. Leget, MD
Nancy C. Lehman, MD
Eric J. Lescault, DO
Daniel R. Lewis, MD
Jonathan L. Lin, MD
Kanhka Linthavong, MD
Peter M. Lipscomb, MD
Jennifer Lira, MD
Allison K. Little, PA-C
Charles W. Lomax, MD
Otis M. Lowry, MD
L.D.A. C. Luvis, MD, FACP
Yvonne Luyando, MD
William D. Lyday, MD
Kimberly G. Lykins, DO
Nchimunya M. Maambo, PA
Henry J. MacDonald, Jr., MD
Mary T. MacKenzie, MD
Jerome J. Magolan, Jr., MD
Ureena Manandhar, MD
Wissam B. Mansour, MD
R. Wade Markham, MD
James W. Markworth, MD
Bernard A. Marshall, MD
Dennis L. Martin, MD
Tiffany Marum, MD
Jordan S. Masters, MD
Michael J. Masters, MD
Emmett C. Mathews, Jr., MD, FACC, FACP, FAHA
Kimberly R. Maurer, MD
A. Thomas May, III, MD
Ronald B. May, MD, FAAP
David B. Maybee, MD
David W. McAllister, MD
Jane H. McCaleb, MD
Chad M. McCall, MD, PhD
Robert J. McCammon, MD
Keith L. McCormick, MD
Kimberly A. McCrea, MD, FCCP
John T. McElveen, Jr., MD
Damian F. McHugh, MD, FACEP
Anjanette L. Mcilwain-McCollum, MD, FAAP
Karin R. McLelland, MD
Julian E. C. McLeod, PA-C
Steven J. McMahon, MD
John T. McMurtry, MD
Wendy W. McNeill, MD
Victor A. Medina, MD
Joan N. Meehan, MD
Milap P. Mehta, MD
John J. Meier, IV, MD
Frank M. Melvin, MD
Roman G. Melvin, MD
H. Curtiss Merrick, MD, FACP
David F. Michael, MD
J. Lloyd Michener, MD
R. Alden Milam, IV, MD
Edith H. Miller, MD
Maxwell S. Miller, DO
Sarah J. Mills, MD
Megan E. Milne, MD
Americo M. Minotti, MD
C. Brent Mizelle, MD
Linda C. Mohr, MD
Gregory J. Mohs, MD
John L. Monroe, MD
Robert W. Monteiro, MD
Daniel H. Moore, MD, FACOG
Alan L. Morgan, MD
Robert G. Morgan, Jr., MD
Jacqueline H. Morris, DO
Artus M. Moser, Jr., MD
Amir R. T. Motameni, MD
Jon Mugweru, MD
Joseph L. Murad, MD
Daniel W. Murphy, MD
Katherine A. Murphy, PA-C
Kelly R. Murphy, MD
Mark T. Murphy, MD, FACC
Richard J. Murphy, MD
Sean J. Murphy, DO
Joanna D. Murray, PA
Holly C. Musgrove, MD
Matthew B. Myers, MD
Keith V. A. Nance, MD
Myra Flor Nario, PA-C
Rushi K. Nayak, MD
Charles R. Neal, MD
William A. Nebel, MD
David S. Nelson, MD
Edwin C. Newman, III, MD
Rosemarie C. Newman, MD, FACOG
Gregory S. Nichols, DO
Peter J. Noone, MD
Mary C. Notaro, DO
Charles F. O'Cain, MD
Michael J. O'Connell, DO
Brian P. O'Donnell, MD, FAAP
Ambrose S. Okonkwo, MD
John G. Oliver, MD
Michael R. Oswald, MD
Harold P. Overcash, MD, FAAP
Carroll C. Overton, MD
Alexander T. Page, MD
Branson H. Page, MD
Hannah M. Palko, PA-C
John A. Papalas, III, MD
Kenneth S. Papier, DO
Pankaj N. Parikh, MD, FACC
Danna M. Park, MD, FAAP
Eunee K. Park, MD
Robert I. Park, MD
Danielle E. Parrish, PA-C
James S. Parsons, MD
Amish V. Patel, MD
Beena N. Patel, DO
Sanjay A. Patel, MD
William R. Patton, MD
Alfredo L. Pauca, MD
Matthew W. Payne, MD
James V. Perciaccante, MD
Jasper B. Perdue, Jr., MD
Henry T. Perkins, Jr., MD
Paul C. Perlik, MD
Everett L. Perry, MD
Jennifer H. Peterson, MD
Noel Peterson, MD
Frederick E. Pfeiffer, MD
Linda C. Pham, PA-C
Dana P. Piasecki, MD
Noah R. Pierson, MD
Harold C. Pillsbury, III, MD, FACS
Holly T. Pilson, MD
Joseph K. Piscitello, MD
Stuart W. Point, MD
Denise Poland-Torres, PA-C
A. Shaye Polk, PA-C
Stewart M. Polsky, MD
William L. Pomeroy, III, MD
Matthew A. Popa, MD
James R. Post, MD
James B. Powell, II, MD
Kothai Divya Pragatheeshwar, MD
James E. Pugh, Jr., MD
Amitabh Purohit, MD
Shrinivas Rajagopalan, MD, PhD
Jennifer L. Raley, MD
R. Pinkney Rankin, Jr., MD
Michael P. Ransone, MD
Tayyabah Rayyast, PA-C
Kelsey L. Rea, PA-C
Kelly K. Redden, DO
Lloyd F. Redick, MD
F. Ed Reedy, Jr., MD, FAAP
Steven H. Reid, MD
Caroline E. Reinke, MD
Donald P. Renaldo, MD
Christopher R. Reynolds, MD, FACEP
Jonathan C. Riboh, MD
Anne S. Richardson, MD
Michael A. Richman, MD
Scott C. Rissmiller, MD
Jesse E. Roberts, MD
Leroy Roberts, Jr., MD, FACR
Stephen C. Robinson, MD
Shannon M. Roche, DO
R. Mark Rodger, MD
David H. Rosenbaum, MD
Michael D. Rosenberg, MD
Elizabeth G. Rossitch, MD
R. Kyle Rothman, MD
Michael C. Rowland, MD
Alethea Y. Rucker, MD
Kathleen R. Ruddiman, DO
Roberto Rupcich, MD
Jarmella P. Russell, MD
Jeffrey K. Russell, MD
William J. Rutledge, MD
Philip R. Saba, MD
Barbara E. Salamon, MD
David L. Saliba, II, MD
M. A. Samia, MD
James R. Sancrant, Jr., DO
Daniel R. Scanga, MD
Charles W. Scarantino, MD, PhD
Richard J. Schneider, MD
Lisa C. Scott, MD
E. James Sebold, MD
Ashish P. Shah, MD
Christopher T. Shah, MD
Hadley J. Sharp, MD
Traci E. Sheaffer, MD
Steffany B. Shearer, DO
Mary D. Shearin, MD
Robert E. Shepherd, MD
Richard H. Shereff, MD
Roger D. Shetterly, MD
Frank W. Shields, IV, MD
Wright D. Shields, MD
J. Daniel Shoffner, MD
Steven A. Siciliano, MD
Leah M. Sieren, MD
David W. Sillmon, MD
Marshall A. Silverman, MD, FACP
Wendy W. Simmons, PA-C
Douglas K. Slater, MD
Andrew J. Smith, MD
David L. Smith, MD
Heatherly M. Smith, PA-C
Henry L. Smith, II, MD
Ian M. Smith, PA-C
S. Keith Smith, MD
Timothy T. Smith, DO
T. Truett Smith, Jr., MPAS, PA-C
Mona M. Soliman, MD
Jessica Son, MD
David R. Sopko, MD
Stephen C. Sorsby, MD
Gwyneth A. Spaeder, MD
Tiffany M. St. Clair, MD
Carey V. Stabler, MD
Walter J. Steele, MD
William R. Stetler, Jr., MD
Amanda R. Steventon, MD
William L. Stewart, MD, FAAP
Christopher A. Stiff, MD
Russell B. Stokes, MD
Michael W. Stratemeier, MD
Christopher T. Stuart, MD
Geeta Subramaniam, MD
Slade A. Suchecki, DO
Jeffrey M. Suchniak, MD
Sang H. Suh, MD
Chasity N. Sullivan, PA-C
Emily X. Sun, MD
Yun Sun, MD
Shane M. Sundlie, MD
Blythe W. Swaim, PA-C
Jason A. Swenson, MD
Bradley M. Swinson, MD
Danielle M. Sykes, PA-C
Shan Tang, MD
Robert B. Tannehill, MD
Muhammad F. Tariq, MD
Eli C. Tate, MD
Barry H. Teasley, MD
Teresa N. Terezis, MD
Alan R. Thalinger, MD
Chanchamma A. Thannikkary, MD
Brian T. Theune, MD
Christopher C. Thomas, MD
David T. Thomas, MD
Alan M. Thomley, MD, FACC
R. Morris Treadway, Jr., MD
Robert C. Turner, MD, FACP
James W. Turpin, MD, MPH
Maria G. Uberti, MD
Jamie Udwadia, MD
Chinazor O. Umerah, MD, MBA, FACP
Ryan C. Vann, PA-C, MHS
Daniel P. Vaughan, MD
William B. Veazey, MD
Ralph N. Vick, MD
Nicholas A. Viens, MD
Keith E. Volmar, MD
Kerri M. Wahl, MD
Aikya F. Waldo, MD
William R. Walker, MD
Kelley Wallace, Jr., MD
Peter A. Wallenborn, III, MD
Stephen L. Wallenhaupt, MD
Yi-Zhe Wang, MD
Patrick L. Ware, MD
John G. Warren, PA-C
Nikunj P. Wasudev, MD
James M. Watson, MD
Polly J. Watson, MD
Samantha S. Watson, MD
Stanley R. Watson, MD
John A. Watts, V, MD
James P. Weaver, MD
Andrew B. Weber, MD
Jade E. Weeks Kimble, PA-C
Michael D. Wehmueller, MD
Jack H. Welch, MD
John A. Welshofer, MD
David R. Wiercisiewski, MD
William D. Wilcox, MD
Geoffrey E. Wile, MD
Robert F. Wilfong, MD
Margaret J. Willhide, MD
Catherine E. Williams, PA-C
Christine A. Williams, PA-C
Martin K. Williams, MD
Noelle L. Williams, MD
Adam K. Willson, MD
Charles F. Willson, MD
Heber G. Winfield, III, MD
Christopher E. Winstead-Derlega, MD
Robert I. Wodecki, MD
Michael R. Wolff, MD
Neil T. Wolfman, MD
Sharon A. Wolters, MD
Jonathan Wons, MD
Terri A. Wood-Cummings, MD
Charles T. Woodham, MD, FACS
Richard H. Wray, III, MD
Thomas H. Wroth, MD
Lawrence R. Wu, MD
Jesse G. Yarborough, Jr., MD
Stephen M. Yeh, MD
Daniel M. Yoder, MD
Judith S. Yongue, MD
Sung-Eun Yoo, MD
Robert K. Yowell, MD
Mark S. Zalaznik, MD
Juozas A. Zavadzkas, MD
Deborah F. Zimmermann, PA-C
NC DHHS to Host RSV, Syphilis, Electronic Birth Registration Webinar

NC DHHS/Division of Public Health, in collaboration with NC AHEC, will be hosting a webinar on Monday, December 4, at 6pm, to provide updates on:
- The launch of new electronic birth registration system
- Congenital syphilis in North Carolina
- RSV vaccination during pregnancy
More information is available at here.
Online registration is available here.
Please share this information with interested colleagues.
Medicaid Redetermination – Physicians Survey

The North Carolina Medical Society has been asked to assist the Center for Medicare & Medicaid Services in ensuring Medicaid patients maintain coverage during the Medicaid redetermination period. CMS is interested in physicians’ experiences in particular.
North Carolina physician feedback would be helpful, and we would be grateful if you would respond to a survey to share your experience and insights. Please reply by Tuesday, December 5th.
Survey questions include:
- What Medicaid unwinding policies/strategies are working well? What is not working well?
- What barriers/ challenges have you faced during the unwinding?
- Are you/your practice working directly with patients to help them maintain Medicaid coverage or to transition to another form of coverage?
- Are you/your practice working with our state’s Medicaid managed care plans (Prepaid Health Plans / PHPs) or other private insurers to help connect patients with coverage options?
If so, what strategies are working well?
- What would be helpful to assist you and your practice in navigating the unwinding and assisting patients with maintaining coverage?
Please feel free to share this notice and survey link with your colleagues.
Thank you for your assistance. Your feedback (excluding your name and contact information) will be shared with CMS.
Secure Your Spot at the NCMS Advocacy Summit!
You're Invited to the NCMS Advocacy Summit!
This groundbreaking event is dedicated to exploring and advancing crucial topics in healthcare. Join us on March 23, 2024, from 9 am to 5 pm at the McKimmon Center, 1101 Gorman Street, Raleigh, NC 27606.
Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering!
Registration is Open! Space is Limited!
NCMS PAC Thankful Thursday!
On this Thankful Thursday, we are recognizing some of our NCMS PAC Investors! Thank you for your continued investment in your patients and profession. Contact Hannah Rice ([email protected]) to learn more about how you can make a difference.
Ashley McKinney, PA-C
Christoph R. Diasio, MD, FAAP
David B. Eddleman, MD
Domenic A. Palagruto, II, DO
James C. Johnson, MD
Marian E. Cranford, PA-C
Shawn Parker
It's Giving Tuesday! Give North Carolinians Access to Care This Year!

During the next 24-hours, people around the world will come together to live out philanthropy – love of humanity – by giving to important causes.
The NCMS Foundation’s important cause is one we suspect is near to your heart too – ACCESS TO CARE.
The Foundation’s piece of this complex puzzle is providing financial incentives and practice support to primary care and behavioral health MDs, PAs and other clinicians as incentive to work in areas of NC that lack sufficient health care professionals and services.
With your help, we can make sure that ALL North Carolinians have an equal chance at healthy lives.
Thank you in advance for your support of the NCMS Foundation!
Polysubstance Abuse Worsening US Opioid Crisis

America's addiction crisis is being ushered into a dangerous new era by rising levels of polysubstance abuse, as more people become addicted to deadly combinations of synthetic opioids and stimulants. The alarming trend is causing concern among addiction specialists and medical professionals, who say the rise of polysubstance abuse is making it harder to treat opioid addiction and taking the crisis to a new, more perilous level.
What is polysubstance abuse?
Polysubstance abuse is described by the U.S. Centers for Disease Control and Prevention (CDC) as the "use of more than one drug." This includes when multiple drugs are taken at the same time or "within a short time period," the CDC explained, "either intentionally or unintentionally." When done intentionally, polysubstance use typically occurs when someone "takes a drug to increase or decrease the effects of a different drug or wants to experience the effects of the combination," the CDC added. Unintentional use happens when someone unknowingly takes drugs that were cut or mixed with other drugs. Either way, the consequences can be deadly because the effects from a combination of drugs "may be stronger and more unpredictable than one drug alone."
Mixing substances is never safe, but combining drugs from opposite drug classes can be especially deadly. Contrary to what some substance users believe, mixing stimulants and depressants "doesn’t balance or cancel them out," the CDC said. "In fact, the results of combining drugs are unpredictable, often modifying or even masking the effects of one or both drugs." This could create the illusion that "the drugs are not affecting you, making it easier to overdose," the agency added.
Continue to the full article here.
Feel the Joy of Giving Back Tomorrow During #GivingTuesday!

Don’t forget to share the love with others on #GivingTuesday!
Tomorrow, as people around the world support important causes, donate to the NCMS Foundation to provide access to NC’s uninsured and under-insured patients.
Your gift will help bring primary care and behavior health MDs, PAs, and other clinicians to mostly rural areas of the state that lack sufficient medical professionals and services, making sure ALL North Carolinians have an equal chance at healthy lives.
Join us in tackling this cause and spread the word to friends and family who also want to make an impact.
Get ready, this #GivingTuesday is going to be a wonderful way to kick off the season of giving!
Energy Assistance Program Helps Older North Carolinians with Heating Costs

The North Carolina Department of Health and Human Services' Low Income Energy Assistance Program will begin accepting applications from older adults and people with disabilities on December 1, 2023.
The federally funded program helps low-income households with a one-time payment sent directly to their heating vendor to offset the high cost of warming their homes during the cold weather months.
"We know the cost of most things are increasing, and keeping homes warm and safe this winter will be a bigger burden for some of our neighbors," said Carla West, Senior Director for Human Services at NCDHHS. "LIEAP helps ensure North Carolina's older adults and people with disabilities who may be facing a financial hardship have the funds to help stay warm throughout these colder months."
Payments will be distributed automatically to heating vendors beginning in December 2023 if a member of the household meets the following three requirements:
- Is age 60 or older or a person with a disability receiving services through the NCDHHS Division of Aging and Adult Services,
- Currently receives Food and Nutrition Services and
- Received a LIEAP payment during the 2022-2023 season.
Households meeting the requirements for the automatic payment will be notified of their eligibility in November 2023 and do not need to re-apply for LIEAP.
Any household with a person 60 or older or with a disability and is receiving services through the Division of Aging and Adult Services who did not receive notice of an automated payment, can apply online at epass.nc.gov. Applicants can also call their county department of social services to apply by phone, in person or print a paper application from epass.nc.gov to mail, fax or drop off at their county department of social services.
To be eligible for the LIEAP program, a household must:
- Have at least one U.S. citizen or non-citizen who meets the eligibility requirements,
- Have income equal to or less than 130% of the federal poverty limit, and
- Be responsible for their heating cost.
Beginning January 2, 2024, all other eligible households who meet the eligibility requirements may begin applying. Applications will be accepted from January 2, 2024, to March 31, 2024, or until funds are exhausted.
Last year, the LIEAP program provided approximately $63 million to help more than 143,000 households pay their heating bills from December 2022 through March 2023. For more information on the program and eligibility, visit here.
New Tribal Affiliation for American Indians on Birth and Death Certificates in NC

The North Carolina Department of Health and Human Services is taking steps to modify the representation of tribal affiliation on birth and death certificates.
"The department is committed to presenting the accurate representation of all people on vital records," said NCDHHS Chief Health Equity Officer and Deputy Secretary for Health Equity, Debra Farrington. "We appreciate the collaborative efforts with the American Indian community and the North Carolina Commission on Indian Affairs to develop these changes to birth and death certificates."
Effective August 28, 2023, all death certificates registered or amended in the North Carolina Database Application for Vital Events (NCDAVE) Electronic Death Registration System and issued by NCDHHS Office of Vital Records include the following race and tribal affiliation options for decedents who identified as American Indian:
- American Indian
- American Indian – Coharie
- American Indian – Eastern Band of Cherokee Indians
- American Indian – Haliwa-Saponi
- American Indian – Lumbee
- American Indian – Meherrin
- American Indian – Waccamaw-Siouan
- American Indian – Sappony
- American Indian – Occaneechi Band of the Saponi Nation
The above options will also be made available for parent(s) race and tribal affiliation for all births registered or amended in the NCDAVE Electronic Birth Registration System and issued by NCOVR beginning January 1, 2024.
According to the 2020 U.S. Census Bureau, more than 130,000 American Indians live in North Carolina, making it the seventh largest American Indian population in the United States.
"This change is long overdue and will help preserve the rich history of American Indian culture in North Carolina," said Rev. Ricky Burnett, Chairman of the NC Commission of Indian Affairs. "The Commission is committed to providing support for and advocating for North Carolina's American Indian population."
Governor Roy Cooper proclaimed November as American Indian Heritage Month, celebrating the history and heritage of the eight state recognized tribes in North Carolina. They are Coharie, Eastern Band of Cherokee, Haliwa-Saponi, Lumbee, Meherrin, Occaneechi Band of the Saponi Nation, Sappony and Waccamaw- Siouan.
Presentation of race and tribal affiliation on birth and death certificates will not impact the state's vital statistics reporting format to the Centers for Disease Control and Prevention National Center for Health Statistics.
More information about birth and death certificates in North Carolina can be found on the website https://vitalrecords.nc.gov.
More information about the NC Commission on Indian Affairs can be found on the North Carolina Department of Administration's website.
You can also learn more about national vital records reporting statistics on the CDC website.
NC Clinician and Physician Retention and Wellbeing Consortium is for YOU!
The North Carolina Medical Society (NCMS), through the North Carolina Clinician and Physician Retention and Wellbeing (NCCPRW) Consortium, aims to address unspoken physical, emotional, and mental areas of stress and burnout.
In 2024, one of the NCMS's priorities focuses on fostering health system environment changes that improve the daily lives of our members through the current and continued work of the NCCPRW Consortium.
The well-being of you, our healthcare clinicians, is not only a moral imperative, but also a fundamental necessity for the effective delivery of healthcare services.
As you all tirelessly work to save lives and provide comfort to those in need, it's essential that we prioritize your physical, mental, and emotional health. Visit the NCMS’s Wellness and Resilience page for additional resources to combat stress, burnout, clinic fatigue, and more.
In addition, there is a free Physician Support Line open Monday – Friday: 8AM – 12 AM ET at 1-888-409-0141, available to clinicians in need of an outlet, resources, or additional support.
Give the Gift of Leadership This Holiday Season! 🎄
Support the next generation of clinicians and aspiring leaders in health care!

Are you interested in making a meaningful contribution to the future of healthcare leadership? Consider becoming a sponsor for a student in the Future Clinician Leadership Course (FCLC) or a scholar in our esteemed Leadership College or Health Care Leadership & Management programs.
- Future Clinician Leadership Course (FCLC): By sponsoring a student in FCLC, you'll empower the next generation of clinicians to develop critical leadership skills early in their careers.
- Leadership College: Sponsorship for Leadership College scholars allows you to directly invest in individuals who are committed to shaping the future of healthcare leadership.
- Health Care Leadership & Management (HCLM): By sponsoring a scholar in HCLM, you'll be supporting healthcare professionals on their journey to becoming visionary leaders. Your contribution can help them drive innovation and improve healthcare delivery.
Why Sponsor? Your sponsorship goes beyond the financial aspect: It's a chance to nurture talent, inspire ambition, and foster the growth of leaders who will impact the healthcare industry positively.
Get Involved Today: To explore sponsorship opportunities and learn more about how you can make a difference in the lives of these emerging leaders, please reach out to Pam Highsmith, VP of Development at [email protected]. Your generosity will play a pivotal role in shaping the future of healthcare leadership.
Join us in our mission to empower the leaders of tomorrow and continue the legacy of excellence that defines the KIPL community. Together, we can make a profound difference in healthcare leadership.
Consider a sponsorship today. It's the gift that keeps on giving!
WCMS Hosts Historical Performance Where Past and Present Come Together
On Sunday November 19th, the Wake County Medical Society hosted a family event at Haywood Hall and Gardens in Raleigh, welcoming highly acclaimed veteran historical actor-interpreter Bill Barker, described as the nation's foremost interpreter of Thomas Jefferson.
Combining the tools of theater with rigorous historical scholarship, Barker explored Jefferson’s life and times, and how it relates to our world today.
7 More Days Until Giving Tuesday! Make Your 2024 Donation Plan Now!
After the back-to-back days of deals on Black Friday and Cyber Monday, join us in kicking off the holiday giving season on #GivingTuesday!

On the Global Day of Giving, we’re raising funds to improve the health and well-being of North Carolinians.
We want to be sure that ALL North Carolinians have an equal chance at healthy lives, and your involvement is essential.
Ways to gear up for #GivingTuesday:
- Donate. Lock in your gift now!
- Follow us on Facebook, Twitter and Instagram
- Share this message and our social media posts and encourage others to join the movement
We’ve got just one week left until the historic day of giving! Let’s do this!
Tips to Help Avoid Norovirus this Holiday Season
While Norovirus outbreaks can happen anytime, they usually occur from November to April. The virus spreads easily and quickly from infected people to others and through contaminated foods and surfaces. People of all ages can get infected and sick.
Taking a few precautions can help protect against the virus:
- Wash your hands often
- Rinse fruits and vegetables
- Cook shellfish thoroughly
- Stay home when sick and for two days after symptoms stop
- Avoid preparing food for others when sick and for two days after symptoms stop
The most common symptoms of Norovirus are diarrhea, vomiting, nausea, and stomach pain.
Learn more about Norovirus here.
Download a Norovirus Fact Sheet here.
Mark Your Calendar Now! Collaborative Care Model Learning Collaborative Planned for Early 2024
Collaborative Care Model (CoCM) Provider
Learning Collaborative
January 18, February 15, March 21, April 18, May 16, June 20, 2024
12:30 - 1:30 p.m. | Location: Livestream Webinar

The Collaborative Care Model (CoCM) is an integrated modality that provides patients with medical and behavioral health care in a primary care setting. The CoCM Learning Collaborative sessions will highlight collaborative care team integration and the role of the CoCM Behavioral Health Care Manager for practices new to the model and those established with implementing CoCM.
Objectives:
- Participants will be able to describe the principles of the Collaborative Care Model (CoCM).
- Participants will be able to identify key concepts and team member roles/responsibilities for effective implementation of CoCM.
- Participants will be able to explain the value and evidence for measurement-based, treatment to target CoCM care.
- Participants will be able to discuss the contributing factors to successful Collaborative Care implementation.
Target Audience:
These Learning Collaboratives are for primary care providers, behavioral health professionals, and anyone else who has implemented or is considering the Collaborative Care Model (CoCM) for integrating behavioral health in a primary care setting. Independent primary care practices, FQHC’s, and rural health clinics may find this collaborative especially helpful for meeting some of the behavioral health needs of their patients.
January 18, 2024 • 12:30 - 1:30 p.m.
Overview of CoCM Model/Role of PCP
February 15, 2024 • 12:30 - 1:30 p.m.
Role of the Psychiatric Consultant/Systematic Caseload Review
March 21, 2024 • 12:30 - 1:30 p.m.
Role of BH Care Manager/Registry Tracking
April 18, 2024 • 12:30 - 1:30 p.m.
CoCM Billing
May 16, 2024 • 12:30 - 1:30 p.m.
Communicating about CoCM Across the Care Team
June 20, 2024 • 12:30 - 1:30 p.m.
Caseload Management/Relapse Prevention Plan
 Registration is required for each date via the link (participants will use this link for each session).
Registration is required for each date via the link (participants will use this link for each session).
Download the PDF here.
For Additional information about the model please click this link.
Questions? Contact LaShawnna Andrews, MSM, Director, Continuing Professional Development IPE at (910) 678-7319 or [email protected]
In Memoriam: Former Wake County Medical Society Executive Director Paul B. Harrison
Paul B. Harrison, former Wake County Medical Society Executive Director, died Tuesday, November 14. He was 79.
Harrison served 21 years as the Executive Director of the Wake County Medical Society (WCMS). In the role, he worked to advance the WCMS mission of developing a medical care safety net for indigent residents of Wake County.
In 2021, Harrison's years of service to the Wake, and surrounding medical communities, were recognized with the John Huske Anderson Award, given annually to a layperson whose contributions have had a positive impact on the medical profession and public health.
Volunteerism became a big part of Paul’s life, with a focus on the least advantaged in our society. He served in the U.S. Peace Corps (Micronesia) and on the staff of the Peace Corps Agency in Washington, DC. In the Triangle, he served as a volunteer innkeeper at the Durham Ronald McDonald house, as a volunteer swim instructor for handicapped students in Chapel Hill, as a volunteer intake screener at the Wake County Open Door Clinic, and as a member of the boards of Urban Ministries of Wake County, The Triangle Community Foundation and Judea Reform Congregation in Durham.
Chip Baggett, CEO of the North Carolina Medical Society (NCMS) had this to say about Harrison: “It is rare to find a public servant who quietly goes about planting and nurturing the seeds of change. Paul’s contribution to the health and well-being of patients is enduring. I am grateful for his leadership.”
The North Carolina Medical Society extends its deepest sympathy to Harrison's family and friends.
Read Harrison's full obituary here.
CDC Warning: Invasive Tick Species Found In NC
Asian longhorned ticks have been found in 19 states, including North Carolina


According to researchers, this invasive species can reproduce quickly, hide in tall grass and survive harsh conditions.
Luckily, compared to other well-known native ticks, the Asian longhorned tick appears to be less attracted to human skin, but have been found on people and also pets, livestock, and wildlife.
Three cows in Ohio died after being bitten tens of thousands of times, promoting the CDC warning. An analysis published in the Journal of Medical Entomology reveals that scientists gathered nearly 10,000 ticks in around 90 minutes at the cow pasture.
The ticks "are light brown in color and are very small, often smaller than a sesame seed," according to the USDA Animal and Plant Health Inspection Service website, which also explains that female Asian longhorned ticks can reproduce without a male, and that "it only takes a single tick to create a population in a new location."
Many species of ticks live in the United States. Each one can carry and spread different types of germs.
When a scientist discovers a new germ in a tick, studies are needed to determine if the tick can carry and spread germs to a person or animal.
A recent experimental study found that this tick is not likely to contribute to the spread of Lyme disease bacteria in the United States, while another laboratory study found that this tick has the ability to carry and spread the bacteria that causes Rocky Mountain spotted fever (Rickettsia rickettsii), though the germs that cause Rocky Mountain spotted fever have not yet been found in these ticks in nature.
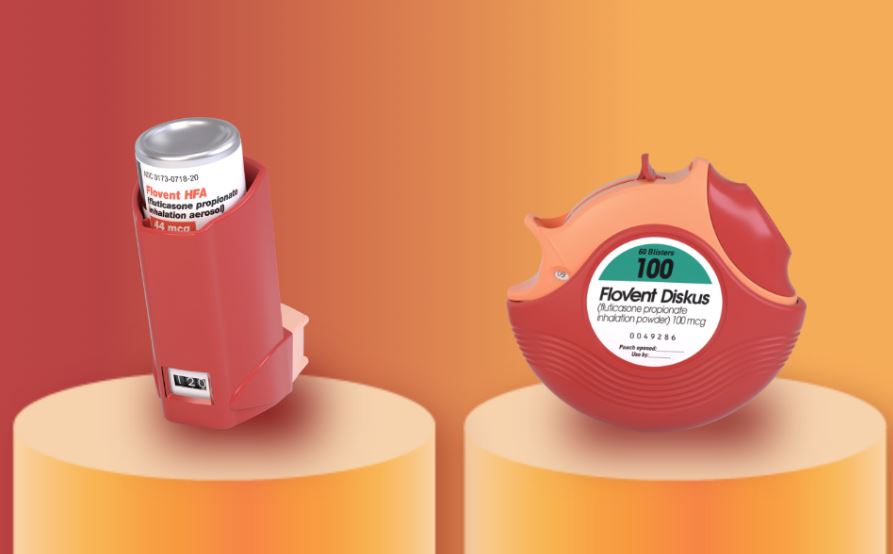
Discontinuation Notice: Flovent HFA and Flovent Diskus

On December 31, 2023, GSK will discontinue all strengths of Flovent HFA and Flovent Diskus. The authorized generics, fluticasone propionate HFA (generic for Flovent HFA) and fluticasone propionate diskus (generic for Flovent Diskus), will be added as preferred on the NC Medicaid Preferred Drug List (PDL) effective December 1, 2023.
According to the FDA, an authorized generic is an approved brand name drug that is marketed without the brand name on its label. Other than the fact that it does not have the brand name on its label, it is the exact same drug product as the branded product. Pharmacies can substitute the generic without an updated or new prescription. However, if an existing prescription for Flovent indicates brand medically necessary or dispense as written, the prescriber will need to provide a new prescription without that requirement so that the substitution is allowed.
Flovent HFA/Diskus will remain preferred so that claims will continue to pay until any remaining stock of the brand is depleted. (source)
Helping New Mothers! National Maternal Mental Health Hotline is Ready in English and Spanish.
24/7, free, confidential hotline for pregnant and new moms in English and Spanish
Pregnancy and a new baby can bring a range of emotions. Many new moms feel overwhelmed, sad, anxious, or exhausted at different times during their pregnancy or after the baby is born. The National Maternal Mental Health Hotline can help, providing 24/7, free, confidential support before, during, and after pregnancy.
The Hotline offers callers:
- Phone or text access to professional counselors
- Real-time support and information
- Response within a few minutes, 24 hours a day, 7 days a week
- Resources
- Referrals to local and telehealth providers and support groups
- Culturally sensitive support
- Counselors who speak English and Spanish
- Interpreter services in 60 languages
Call or text the National Maternal Mental Health Hotline: 1-833-TLC-MAMA (1-833-852-6262). TTY users can use a preferred relay service or dial 711 and then 1-833-852-6262.
Frequently Asked Questions about the National Maternal Mental Health Hotline.
The hotline also offers a Partner Toolkit for health care organizations to help raise awareness.
ECU Rural Family Medicine Residency Program Bringing Health Care to Underserved Communities
East Carolina University’s Brody School of Medicine and ECU Health launched a new Rural Family Medicine Residency Program in 2021 that equips physicians with specialized training in caring for patients in rural and underserved communities.
The program is designed to give recent medical school graduates interested in serving as family medicine physicians in rural communities first-hand experience in caring for patients in the kind of under-resourced settings they plan to practice in upon completion of their residency training.
The residents spend a majority of their first year of training at ECU Health Medical Center in Greenville. They then spend the next two years training in either the rural Hertford County community of Ahoskie — at the Roanoke Chowan Community Health Center and ECU Health Roanoke-Chowan Hospital — or in Duplin County at Goshen Medical Center in Beulaville and ECU Health Duplin Hospital in Kenansville.
The program exposes the residents to the breadth of family medicine — in both resource-abundant academic medical center environments and resource-scarce rural environments — so they are well-prepared to provide comprehensive care in a variety of practice settings.
While in the rural communities, the residents build connections with their patients and become integrated into the communities they serve.
Read more about the Rural Family Medicine Residency Program and their unique approach to training physicians here.
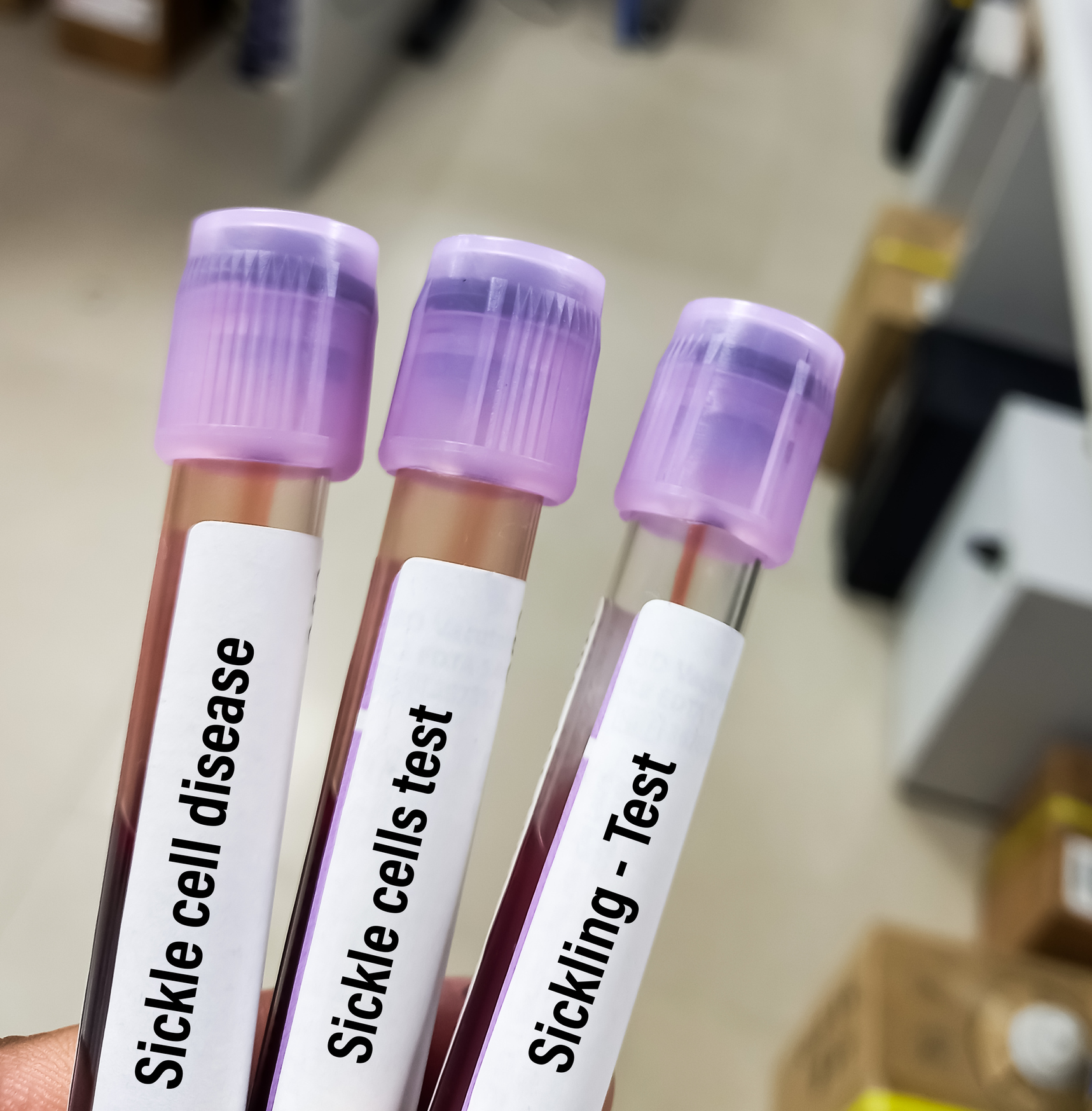
Gene Therapy for Sickle Cell Disease Approved in UK. What Could this Mean for US?
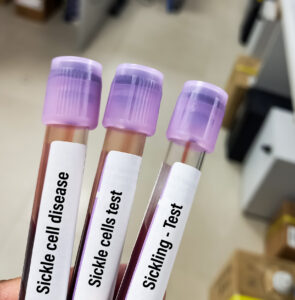
LONDON – Britain's medicines regulator has authorized the world's first gene therapy treatment for sickle cell disease, in a move that could offer relief to thousands of people with the crippling disease in the U.K.
In a statement on Thursday, the Medicines and Healthcare Regulatory Agency said it approved Casgevy, the first medicine licensed using the gene editing tool CRISPR, which won its makers a Nobel prize in 2020.
The agency approved the treatment for patients with sickle cell disease and thalassemia who are 12 years old and over. Casgevy is made by Vertex Pharmaceuticals (Europe) Ltd. and CRISPR Therapeutics. To date, bone marrow transplants, extremely arduous procedures that come with very unpleasant side effects, have been the only long-lasting treatment.
“The future of life-changing cures resides in CRISPR based (gene-editing) technology,” said Dr. Helen O'Neill of University College London.
“The use of the word ‘cure’ in relation to sickle cell disease or thalassemia has, up until now, been incompatible,” she said in a statement, calling the MHRA's approval of gene therapy “a positive moment in history.”
Learn more about this first-of-its-kind approval here.
WHO Makes Loneliness a Global Health Priority
"It is an 'underappreciated' threat to health that has now become widespread."

CNN — The World Health Organization is making loneliness a global health priority, it said Wednesday, launching a new Commission on Social Connection.
For the next three years, the commission will focus on ways to address the “pressing health threat” of a global epidemic of loneliness, reviewing the latest science and designing strategies to help people deepen their social connections. It’s co-chaired by African Union Youth Envoy Chido Mpemba and US Surgeon General Dr. Vivek Murthy, who has written and spoken extensively about the risks of social isolation and has made the issue one of his top concerns while in office.
According to one survey almost a quarter of the world feels lonely. Gallup says nearly one in four people worldwide -- which translates into more than a billion people -- feel very or fairly lonely, according to a recent Meta-Gallup survey of more than 140 countries.
Notably, these numbers could be even higher. The survey represents approximately 77% of the world’s adults because it was not asked in the second-most populous country in the world, China.
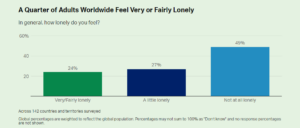
Continue to the full article from CNN here.
Continue to the full article from Gallup here.
NCDHHS: Historic Medicaid Reimbursement Rate Increases Coming Soon. Who Will be Impacted?
RALEIGH -- The North Carolina Department of Health and Human Services (NC DHHS) announced historic Medicaid reimbursement rate increases will soon be implemented for most mental health, substance use, intellectual and developmental disabilities (I/DD) and traumatic brain injury (TBI) services in North Carolina. This transformative change is the first increase to the state minimum reimbursement rates for behavioral health services in more than a decade. Raising these rates will strengthen the care workforce who provide these services and increase access to care for every North Carolinian. It will also make Medicaid expansion more impactful for the estimated 600,000 people who will gain access to these Medicaid health care services.
"These rate changes are a lasting and transformational investment in behavioral health services and whole-person care in North Carolina," said NCDHHS Secretary Kody H. Kinsley. "This will improve the foundation of care so every child and adult can get the necessary mental health and substance use disorder treatment when and where they need it."
The behavioral health care crisis impacts everyone in the state — one in four children and one in five adults are experiencing a mental health need. Rates of anxiety and depression have skyrocketed in recent years, and providers of care have been hard-pressed to keep up. There are dozens of counties in North Carolina that lack a psychiatrist and each day in North Carolina, more than 300 adults and children are waiting in emergency departments for a behavioral health care bed.
"For many, the introduction to behavioral health care is through the crisis system and hospital emergency departments,” said Kelly Crosbie, the Director of the NCDHHS Division of Mental Health, Developmental Disabilities, and Substance Use Services. "We must improve access to routine mental health care and substance use treatment in every North Carolina community, so services are available when people need them."
"The old reimbursement rates are inadequate; meaning, behavioral health practitioners, including psychiatrists, can’t cover the costs of providing care to individuals covered by Medicaid," said Dr. Carrie Brown, NCDHHS Chief Psychiatrist. "This change will help to recruit and retain more behavioral health providers, including physicians, psychologists and other licensed professionals like clinical social workers, into the public behavioral health system in North Carolina, which is critical to ensuring access to care for all North Carolinians, regardless of the health care payer."
NCDHHS received a significant investment in behavioral health care services in the 2023-2025 approved budget. A total of $835 million in one-time and recurring funds was appropriated which represents the single largest investment in behavioral health by the state legislature. Among other things, this critical funding will increase Medicaid payment rates to 100% of Medicare for applicable services like outpatient and inpatient behavioral health services and provide inflation-based increases for most enhanced behavioral health services that do not have a Medicare equivalent. For example, the overall reimbursement for inpatient behavioral health services is expected to increase by 30%. And psychiatric diagnostic evaluation will almost double from the prior rate. All of the Medicaid behavioral health rate increases will be effective for services provided on or after January 1, 2024. Additional information on these increases will be shared through a Medicaid Provider Bulletin.
To ensure adequate access to treatment and support services, many of which help prevent crises, rate funding for diagnostic evaluations and developmental/psychological testing and evaluation will also be increased above the Medicare rate, pending CMS approval. Rates for enhanced substance use disorder services and residential substance use disorder services have either recently been updated or are under consideration for potential increases in 2024 as part of a separate effort related to the NCDHHS 1115 SUD Institution for Mental Disease Demonstration waiver.
The 2023-2025 budget also allows for substantial investments in alternatives to the emergency department such as facility-based crisis services and investments in direct support professionals, including peer support professionals, who are the backbone of any functioning behavioral health, I/DD and TBI care system.
These rate increases will have a positive impact on the more than 2.3 million people served by Medicaid in allowing increased access to behavioral health services and leads the way for other employers and insurers to continue making similar investments. (source)
Wild and Weird Biology: Have Scientists Discovered the First "Vampire" Virus?

In March 2020, Tagide deCarvalho saw something truly strange - something she thinks no other scientist has ever seen before: a virus with another, smaller virus latched onto its "neck." The backstory of this viral attachment is like a master class in how wild and weird biology can be.
The two microbes are both bacteriophages, viruses that infect bacteria, that were harvested from a clump of dirt in Poolesville, MD. Bacteriophages, also called simply phages, are among the most abundant organisms on Earth. There can be millions in a gram of dirt.
But with a special kind of microscope that uses a beam of electrons to capture images, deCarvalho witnessed a truly bizarre moment - kind of like a wildlife photographer who captures an animal behavior that no one had anticipated.
"I could see literally hundreds of them had this little guy attached at the neck, and it was clearly not random," said deCarvalho, who manages the Keith R. Porter Imaging Facility at University of Maryland at Baltimore County. "We know that viruses can do some amazing, interesting things. But this is just another new thing that no one could have predicted we would see."
In a recent study in the Journal of the International Society for Microbial Ecology, deCarvalho and colleagues explain how the viral odd couple likely came to be. The small virus, called MiniFlayer, lost the ability to make copies of itself inside cells, which is how viruses reproduce. So evolution devised a clever, parasitic workaround. MiniFlayer takes advantage of another virus, dubbed MindFlayer, by grabbing onto its neck, and when they enter cells together, MiniFlayer utilizes its companion's genetic machinery to proliferate.
Is it an embrace? A stranglehold? DeCarvalho compares the relationship to viral hitchhiking. Her collaborator, Ivan Erill, a computational biologist at UMBC, likens it to a vampire sinking its teeth into its prey. It's not a perfect analogy, but he notes that sometimes, when they find MindFlayer alone, they can find "bite marks" where MiniFlayer's tendrils were attached.
"Viruses will do anything. They are the most creative force of nature," Erill said. "If anything is possible, they will come up with a way to do it. But no one had anticipated that they would do something like this."
The strange universe of viruses
The discovery started with an undergraduate class designed to teach students basic laboratory techniques, asking them to isolate phages from soil samples and study them using genetics. DeCarvalho has been working with the program for seven years and says that for many of the students, seeing the phage is an exciting moment, like when expecting parents see the ultrasound of a fetus for the first time.
In this case, undergraduates Jenell Lewis and Hira Ahmed isolated and named their phage MindFlayer in 2019. But genome sequencing returned puzzling results, suggesting some kind of contamination. When deCarvalho looked at it with a microscope, she noticed not one phage, but two.
The "virosphere," as scientists call the strange universe of viruses, is known to include elements called "satellites" that have lost their ability to replicate inside cells. Usually, satellites overcome this deficiency by integrating into the genome of the cells that they infect. They lurk there until another virus, a "helper" that has the missing ingredients, happens to enter the cell. The satellites then seize the opportunity to make copies of themselves.
MiniFlayer is a satellite, but unlike the typical version, it doesn't have the ability to hide inside cells. That leaves it with a conundrum: How to make sure it ends up in the cell with its helper at the same time.
"What this virus has done is say, okay, I'm going to attach to my helper, attach to its neck - and travel with my helper until we find a new cell," Erill said.
This is par for the course in microbiology, where tactics like molecular piracy and hijacking have been honed over millions of years of evolution. Bacteria are wildly outnumbered by their viral predators, putting them in an ongoing evolutionary arms race. Bacteria develop defenses, and viral phages develop counter-defense strategies. Phages parasitize other phages.
Researchers are interested in using phages, the natural predators of bacteria, as medicine. Phage therapy can be used to target harmful infections, an approach that could become more important as antibiotic-resistant bacteria have become a growing threat.
Terje Dokland, a microbiology professor at the University of Alabama at Birmingham who was not involved in the study, said the observation of the two attached phages was "intriguing" but called for more images and research to draw firmer conclusions about the interaction, and to tease out whether the two viruses are really co-infecting cells.
The authors hope to collaborate with groups that use a different form of electron microscopy to understand what's happening more clearly. Unlike a vampire, deCarvalho points out, the MiniFlayer isn't sucking something out of MindFlayer.
"We don't know whether or not the satellite is injecting its DNA into the helper or if it's just hitchhiking along for a ride and then falling off, like a tick," deCarvalho said. "Hopefully someone else will pick up this work and figure out that really interesting question." (source)
Grifols Receives FDA Expansion Approval at North Carolina Site

Grifols, a global leader in plasma medicines, announced it has received approval from the U.S. Food and Drug Administration (FDA) for its new immunoglobulin (Ig) purification and filling facility at its Clayton manufacturing campus, one of the world’s largest sites for producing plasma-derived medicines.
The FDA approval is for Gamunex®-C, a leading Grifols Ig brand. This enables the company to manufacture an additional 16 million grams of the therapy annually, bringing total global capacity to 60 million grams. Soon Grifols will seek FDA authorization for the new plant to also produce XEMBIFY®, its quickly growing subcutaneous Ig.
Patient need for Ig therapeutics is expected to rise, especially to treat the growing prevalence of immunodeficiencies, which account for approximately 40% to 55% of the total Ig market, according to the company.
Purification and filling follows the fractionation of plasma into separate proteins, including Ig, alpha-1 proteinase inhibitor, albumin and antithrombin-III, each indicated for different conditions. It is the last step before finished medicine vials are packaged and shipped.
Grifols Engineering engineered and built the new 150,000-square-foot, Green Globes®-certified purification and filling facility.
It is the most recent expansion of Grifols’ flagship Clayton plasma-medicine manufacturing campus.
As it approaches its 50-year anniversary in 2024, the site has evolved into a global showcase for the advanced manufacturing of hemoderivatives.
Over the last decade, Grifols has invested approximately USD 1 billion in the site, including a new plasma fractionation building that began production in early 2022 and increases the site’s overall fractionation capacity to 12 million liters/year, more than half of the company’s global total.
“Having achieved FDA approval earlier than expected for our new purification and filling plant, Grifols continues investing in new technology and expanding our plasma-medicine manufacturing capabilities to address the growing need for immunoglobulins and other plasma-protein therapeutics,” said Victor Grifols Deu, Grifols Chief Operating Officer. (source)
Lung Cancer Report Shows Troubling Statistics for North Carolina

The American Lung Association in North Carolina released its 2023 “State of Lung Cancer” report, which finds that the incident rate of lung cancer cases in the state is far too high. North Carolina has 63 new cases per 100,000 people, compared to the national average of 54.6 new cases per 100,000 people. Working to increase lung cancer screenings and early diagnosis is key to addressing the burden of lung cancer in North Carolina.
The 6th annual report highlights the toll of lung cancer in North Carolina and examines key indicators including new cases, survival, early diagnosis, surgical treatment, lack of treatment and screening rates.
While the incident rate of lung cancer cases is too high in North Carolina, the report also finds that the state ranks above average for lung cancer screening and above average for lack of treatment. However, health disparities exist. Asian or Pacific Islander individuals in North Carolina are least likely to be diagnosed early.
“Lung cancer continues to be the leading cause of cancer deaths here in North Carolina and across the nation. Our recent report makes it clear that we have more work to do to increase lung cancer screening and early detection initiatives, as well as address health disparities in our AAPI community,” said Markus Hill, chair of the Lung Association’s North Carolina Board.
The report found that North Carolina ranks:
- 39 out of 48 in the nation for rate of new lung cancer cases at 63.0 per 100,000. The national rate is 54.6 per 100,000.
- 21 out of 42 in the nation for survival at 26.0%. The national rate of people alive five years after a lung cancer diagnosis is 26.6%.
- 26 out of 47 in the nation for early diagnosis at 26.6%. Nationally, only 26.6% of cases are diagnosed at an early stage when the survival rate is much higher.
- 11 out of 51 in the nation for lung cancer screening at 7.1%. Lung cancer screening with annual low-dose CT scans for those at high risk can reduce the lung cancer death rate by up to 20%. Nationally, only 4.5% of those at high risk were screened.
- 28 out of 47 in the nation for surgery at 19.4%. Lung cancer can often be treated with surgery if it is diagnosed at an early stage and has not spread. Nationally, 20.8% of cases underwent surgery.
- 12 out of 47 in the nation for lack of treatment at 17.5%. Nationally, 20.6% of cases receive no treatment.
- 26 out of 51 in the nation for smoking at 14.4%. Nationally, 13.5% of adults currently smoke.
North Carolina became the 41st state (including the District of Columbia) to expand Medicaid to adults with incomes up to 138 percent of the federal poverty level, enacting the move in its 2023-2024 fiscal budget. Beginning December 1, 2023 more than 600,000 low-income children, adults, pregnant individuals, people with disabilities, and seniors will gain access to health care.
Nationally, the “State of Lung Cancer” report finds that lung cancer survival rates are improving for everyone, including people of color. In fact, the five-year lung cancer survival rate for people of color has increased by 17% in the last two years, helping close the health disparity gap.
“Thankfully, nationally, the lung cancer survival rate has improved because of increased awareness, improved access to healthcare and cutting-edge research into new treatments for the disease,” added Hill. “We need to keep up the momentum to save more lives.” (source)
Related Reading:
American Cancer Society Updates Guidelines for Lung Cancer Screenings
Want to get involved and help the mission of the American Lung Association. Register for The Fight for Air Climb – Charlotte. This event takes place March 23, 2024. Learn more and register here.
NC Medicaid Expansion Update: Provider and Member Flexibilities

The Department has policy flexibilities for expansion members and providers treating those expansion members to ensure beneficiaries receive the care they need, while easing provider administrative burden. Unless otherwise noted, the below flexibilities apply to only expansion members.
- Providers can identify expansion members by checking the member’s eligibility in the NCTracks Recipient Eligibility Verification feature in the Category of Eligibility section.
- Expansion members, for whom these flexibilities apply, will have eligibility categories MXPNN or MXPGN listed.
The Provider Factsheet on Medicaid Expansion has more information for providers related to Medicaid expansion.
Please see the below flexibilities for expansion beneficiaries and providers for the launch of Medicaid expansion.
- Medical Prior Authorizations (PA): For medical PAs, between December 1, 2023 and May 31, 2024, health plans will honor existing NC Medicaid medical PAs. Medical PAs are any PA for physical and behavioral health services. This flexibility applies to both in-network and out-of-network providers who are active enrolled NC Medicaid providers.
- Pharmacy PAs: For pharmacy PAs, between December 1, 2023, and May 31, 2024, Standard Plans and NC Medicaid Direct will honor existing pharmacy PAs (from NC Medicaid, as well as other health plans). Previous PAs available as of December 1, 2023, will be honored through May 31, 2024, or for the life of the PA, whichever is longer. Plans may consider previous PAs and current drug therapy when making coverage determinations through May 31, 2024. This flexibility applies to both in-network and out-of-network providers who are active enrolled NC Medicaid providers.
- Expedited PA Requests/Reviews for Expansion Beneficiaries: Health plans are required to implement strategies to minimize disruption of benefits at launch of expansion, specifically related to PAs. Health plans are required to implement processes to allow providers to submit expedited PAs for expansion beneficiaries so that services are not disrupted at transition. This flexibility applies to both in-network and out-of-network providers who are active enrolled NC Medicaid providers.
- Out of Network Provider Rates: In addition to out of network requirements found in the Department’s Transition of Care policy, between December 1, 2023, and May 31, 2024, health plans must reimburse Medicaid-eligible nonparticipating/out of network providers equal to those of in network providers. This means that medically necessary services will be reimbursed at 100% of the NC Medicaid fee-for-service rate for both in- and out- of network providers.
Starting on June 1, 2024, out-of-network providers with whom the health plans have made a good faith effort to contract with, will be reimbursed at no more than 90% of the Medicaid fee-for-service rate. Note: Out of network providers must be enrolled in NC Medicaid to be reimbursed by the health plans. - Out of Network Providers Follow In-Network PA Rules: Between June 1, 2024, and August 31, 2024, health plans will permit uncontracted, out-of-network providers enrolled in NC Medicaid to follow in-network provider PA rules. Starting on Sept. 1, 2024, out-of-network providers must seek authorization for all services.
- Primary Care Provider (PCP) Changes for All Beneficiaries: Between December 1, 2023, and Aug. 31, 2024, all beneficiaries may change their PCP for any reason.
NC Medicaid remains committed to working with provider and health plan partners to verify services are paid for without undue burden to beneficiaries and providers during the launch of Medicaid expansion. Providers who experience issues during this transition period should reach out to the contacts below.
Contact
- For managed care issues: Contact the health plans leveraging the information on the Health Plan Contacts and Resources page.
- For other provider issues: Medicaid Provider Ombudsman at [email protected] or 866-304-7062.
Call for Poster Submissions: 2024 NC Ob/Gyn Society Annual Meeting
NC Society of Obstetrical and Gynecological Society
2024 Annual Meeting
March 8-10, 2024
Marriott City Center - Charlotte
Call for poster abstract submissions: Due February 3, 2024
You are invited to submit a poster abstract to the NC Ob/Gyn Society Annual Meeting. The Annual Meeting will be held over the weekend of March 8-10, 2024, at the Marriott City Center in Charlotte. We hope you will plan to attend!
This year, in addition to our resident oral presentations, we are adding a poster session to facilitate the exchange of ideas between providers and medical communities. Abstracts can be from original research, case reports, safety projects and quality improvement projects. An NC Ob/Gyn Society member must be part of the authorship. Preference will be given to projects involving learners, trainees and those involving inter-professional activities. Abstracts may be presented at other venues or in process for publication. Because we have limited space in our exhibition area, we request a limit of two abstract submissions per author.
Abstract submissions are due February 3, 2024. Please submit abstracts to Megan Eberle ([email protected]) by email as an attached Word document.
Please see the Abstract Submission Requirements and Information, and share this request for abstract submissions with residents, fellows, students, advanced practice providers or other leaders in women’s health care in your community.

Start planning now to attend to the NCOGS's 2024 Annual Meeting. The conference will be held over the weekend of March 8-10 at The Marriott City Center in Charlotte. Make your hotel reservation today online or call directly at (704) 333-9000.
Three NC Cities Rank Best Places to Start a Business

RALEIGH – Raleigh is the best place among the nation’s 100 largest metros and Durham is third, according to a new study from Charlotte-based financial services firm LendingTree.
Charlotte came in second, according to the report issued Tuesday.
Austin, Texas – often seen as Raleigh’s rival as a technology hub – fell to seventh from second.
Among the highlights: Raleigh scored a perfect 100 for business climate and finished with an overall score of 86.5. Charlotte scored 77.1, Durham 76.6.
It’s a repeat honor for Raleigh, which topped the previous LendingTree study in 2021. Charlotte rose one spot as did Durham in the new one.
About Raleigh the report says it “holds solid scores in our three categories — business climate, entrepreneurship and local economy — and places 25th or better in six of the nine individual metrics.”
THE TOP TEN
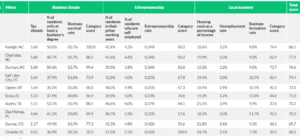
LendingTree pointed out that the “strong business climate score” was due in part to “its high rate of residents 25 and older with a bachelor’s degree or higher — 50.8%, the sixth-highest in our study.”
Raleigh also scored well in entrepreneurship, the number of workers in their “prime working years” and percentage of self-employed residents at 4.2%.
Those numbers increased from the 2021 report, strengthening Raleigh’s grip on the top spot, the study notes:
- Raleigh’s percentage of residents 25 and older with a bachelor’s degree or higher improved to sixth from seventh in our 2021 study.
- Raleigh’s proportion of residents in their prime working years jumped to seventh from ninth in 2021.
- North Carolina ranks 11th in our business survival rate metric — 82.7% of the state’s startups make it past the one-year mark, 1 percentage point above the national average of 81.7%.
Noting that Durham is the 10th smallest in the 100 metros studied, the report pointed out the city ranked “seventh for the percentage of residents with at least a bachelor’s degree (50.6%), just behind Raleigh’s 50.8%.”
However, Durham received “mediocre rankings in our entrepreneurship metrics. It placed 39th for the proportion of residents in their prime working years and 44th for the percentage of self-employed residents — significantly lower than nearby Raleigh, ranked 28th.” (source)
NCMS Member Performs Hospital's First Code STEMI Procedure
WakeMed Cary Hospital now provides advanced cardiac intervention services for patients with ST Segment Elevation Myocardial Infarction (STEMI). This specialized care and response plan for acute heart attacks re-opens blocked coronary arteries, reduces the time to treatment, and improves outcomes for STEMI patients.
The hospital treated its first Code STEMI patient, transported via EMS, on November 2. Dr. Pratik Desai from Cary Cardiology alongside the WakeMed Heart & Vascular Labs support team performed the procedure and re-opened the patient’s artery in 33 minutes.
The American Heart Association and American College of Cardiology recommended “door to balloon” time to treatment is under 90 minutes.

“This new service is beneficial for the residents of Cary, southwestern Wake County and surrounding communities by decreasing the travel time it takes to reach a hospital capable of re-opening blocked arteries and restoring blood flow to damaged heart muscle,” said Doug Trocinski, MD, emergency medicine physician and chief medical officer at WakeMed Cary Hospital. “Time is muscle when it comes to heart attacks, and this service will save lives and improve the quality of life for patients.”
Tech Giant Offers Virtual and In-Person Health Care in North Carolina

In February, Amazon acquired One Medical, which offers in-office and 24/7 virtual care services, on-site labs, and programs for preventative care, chronic care management, common illnesses, and mental health concerns. Now, Amazon is offering these health care benefits to its Prime members.
The One Medical membership is $9 a month (or $99 annually), with the option to add up to five additional memberships for $6 a month each. The membership fee includes access to virtual services at no extra cost, but in-person care or pre-scheduled remote visits will be billed to insurance or paid out-of-pocket.
North Carolina is one of the few states where One Medical is offering in-person services, available in Charlotte and Raleigh-Durham.
“When it is easier for people to get the care they need, they engage more in their health, and realize better health outcomes,” Neil Lindsay, senior vice president of Amazon Health Services, said in a news release on November 8. “That’s why we are bringing One Medical’s exceptional experience to Prime members—it’s health care that makes it dramatically easier to get and stay healthy.”
The new venture is not with scrutiny. The Federal Trade Commission raised privacy concerns.
Learn more about Amazon Health's One Medical here.
Today is World Diabetes Day! NCMS Foundation, AMA Need Your Help to Stop the Spread
More than 1 Million North Carolinians have diabetes
World Diabetes Day provides an opportunity to raise awareness of diabetes as a global public health issue and what needs to be done, collectively and individually, for better prevention, diagnosis and management of the condition.
Every year an estimated 72,032 people in North Carolina are diagnosed with diabetes.
Take a stand against diabetes!
DIABETESFREENC is a joint initiative of the NCMS Foundation and the American Medical Association (AMA) aimed to stop the spread of diabetes in NC.
The National Diabetes Prevention Program (DPP) is a lifestyle change program that has free or low-cost options for patients, regardless of their insurance provider and you can refer using any of these convenient platforms: Our Community Health Initiative (OCHI), NC CARE 360 and the DPP Navigator.
Your pledge demonstrates your willingness to support diabetes prevention in NC! Pledge TODAY!
Lung Cancer Awareness Event Offers Free Screenings and Resources Tuesday
Atrium Health Wake Forest Baptist Comprehensive Cancer Center and Atrium Health Levine Cancer are holding a free lung cancer awareness fair, Tuesday, November 14 from 8 to 11 a.m. at Wake Forest Baptist’s Downtown Health Plaza, located at 1200 N. Martin Luther King Jr. Dr. in Winston-Salem.
The free event is open to all adults, regardless of insurance coverage, income level or immigration status.
One in 16 people will be diagnosed with lung cancer in their lifetime, according to the American Cancer Society. Lung cancer is the deadliest type of cancer for both men and women, and each year, more people die of lung cancer than of breast, colon and prostate cancers combined. That is why screening and early detection is so important.
The Atrium Health Levine Cancer Mobile Screening Unit will be on site and free lung screenings will be offered to individuals who:
- Are between 50 and 80 years of age
- Are uninsured, underinsured or covered by Medicaid
- Have a 20 pack-year smoking history (one pack a day for 20 years or two packs a day for 10 years)
- Currently smoke or have quit smoking within the past 15 years
In addition to the lung screenings, a variety of resources will be offered, including:
- Education on the importance of lung screenings and early detection of lung cancer
- Education on symptoms and treatment for lung cancer
- Resources to assist with smoking cessation
- Opportunities to connect with community organizations
“The goal of this event is to educate our community on the importance of early detection and reinforce our commitment to expanding access to everyone we serve,” said Dr. Jeff Petty, co-leader of the lung cancer program at Atrium Health Levine Cancer and professor of hematology and oncology at Wake Forest University School of Medicine.
“Having the mobile screening unit is such an important tool and we are pleased to offer this opportunity in the Triad for the first time. Wake Forest Baptist is the only NCI-designated Comprehensive Cancer Center in the area, and we are committed to decreasing the burden of cancer in our communities and across the nation.”
For those who require follow-up care, the team will offer onsite counseling that educates patients and ensures they know what care is needed, why it’s needed and how to access this care.
Participants will also receive light refreshments and there will be giveaways.
Those who wish to learn more about the event may call 336-713-3665 or email [email protected].
Join NCMS for 'Making Care Primary' Education Sessions

Earlier this year, the Centers for Medicare & Medicaid Services (CMS) announced that North Carolina is among eight states selected to participate in its Making Care Primary (MCP) practice model initiative.
The innovation effort model seeks to improve care for patients by:
1) expanding and enhancing care management and care coordination,
2) equipping primary care clinicians with tools to form partnerships with health care specialists, and
3) leveraging community-based connections to address patients’ health needs as well as their health-related social needs.
The NC Medical Society, in conjunction with, North Carolina Academy of Family Physicians, NC-AHEC, NC Medical Group Managers Association, and the NC Community Health Center Association will co-host two learning sessions for practices to learn more about the new CMS Innovation Center’s Making Care Primary Model: Monday, November 20th and the national session on Tuesday, November 21st.
Monday, November 20th, at 6 p.m., Nicholas Minter, MPP, Director of the Division of Advanced Primary Care, Patient Care Models Group at the CMS Innovation Center will provide a brief presentation and take questions from North Carolina practices that have applied or plan to apply for the model. Be sure to register here to attend.
Tuesday, November 21st, at 2 p.m., the MCP Team will hold a National Office Hours webinar. In addition to a live Q&A, attendees will be able to submit questions in advance by registering here. Please note, this will be the final Office Hour event before the application portal closes on Thursday, November 30 at 11:59 p.m.
Interested organizations are encouraged to begin their applications even if they are not prepared to submit at this time; doing so helps CMS provide more tailored support to applicants. Eligibility requirements and additional model details can be found in the Request for Applications.
To support application submission, the MCP team has made available the following resources:
- MCP Application example in PDF format
- Recording of last month's Office Hours, as well as a transcript and slides
Additional resources for interested applicants:
- Making Care Primary Model Overview Video and Model Overview Factsheet
- Application Tracks Factsheet, which includes an example decision tree for track selection
- Frequently Asked Questions, which are updated on a rolling basis
- Payer Partner Factsheet and Payer Partners Guide to Alignment
- CMS Innovation Center Primary Care Models Comparison
For questions about the Making Care Primary Model, please reach out to [email protected].
Register Now to Secure Your Spot at the NCMS Advocacy Summit!
You're Invited to the NCMS Advocacy Summit!
This groundbreaking event is dedicated to exploring and advancing crucial topics in healthcare. Join us on March 23, 2024, from 9 am to 5 pm at the McKimmon Center, 1101 Gorman Street, Raleigh, NC 27606.
Don't miss this opportunity to be part of a transformative event. Secure your spot today by registering!
Registration is Open! Space is Limited!
New Addiction Medicine CME Series Helps You Meet Updated DEA Requirements

The North Carolina Medical Board and Wake AHEC, in collaboration with the North Carolina Medical Society and the Addiction Medicine Fellowship program at UNC School of Medicine, have developed an eight-hour CME series that meets the new training requirement recently established by the federal Drug Enforcement Administration (DEA).
On December 29, 2022, the Consolidated Appropriations Act of 2023 enacted a new one-time requirement for active DEA registrants to complete eight hours of education on the treatment and management of patients with opioid or other substance use disorders. DEA registrants who renew on or after June 27, 2023, will be asked to certify that they have completed the required hours.
The new Addiction Medicine Series offers education on a variety of key topics in addiction medicine, including the impacts of stigma, integrating addiction treatment in the primary care setting, and treatment of substance use in special populations.
Here is the full list of classes available in the series:
1. The End of a Bygone Era: Removal of the X-waiver Next Steps in Buprenorphine Prescribing
2. Addiction In Primary Care
3. Treating Chronic Pain and Addictions
4. Responding to Pediatric Substance Use
5. Understanding the Impacts of Stigma: Substance Use Disorder
6. Addiction and Mental Illness
7. The Impact of Stigma and Bias on Substance Use Disorder Diagnosis and Treatment
8. Current State of MOUD Access
Learn more and how to register here.
It's Time for a Healthier NC. Take the Pledge to Stop Diabetes in its Tracks!
November is National Diabetes Month.
Take a stand against diabetes!
DIABETESFREENC is a joint initiative of the NCMS Foundation and the American Medical Association (AMA) aimed to stop the spread of diabetes in NC.
The National Diabetes Prevention Program (DPP) is a lifestyle change program that has free or low-cost options for patients, regardless of their insurance provider and you can refer using any of these convenient platforms: Our Community Health Initiative (OCHI), NC CARE 360 and the DPP Navigator.
Your pledge demonstrates your willingness to support diabetes prevention in NC! Pledge TODAY!
Nearly Half of NC Residents are Obese. Will Newly Approved Drug Help?

The U.S. Food and Drug Administration approved Zepbound (tirzepatide) injection for chronic weight management in adults with obesity (body mass index of 30 kilograms per square meter (kg/ m2) or greater) or overweight (body mass index of 27 kg/m2 or greater) with at least one weight-related condition (such as high blood pressure, type 2 diabetes or high cholesterol) for use, in addition to a reduced calorie diet and increased physical activity. Tirzepatide, the active ingredient in Zepbound, is already approved under the trade name Mounjaro to be used along with diet and exercise to help improve blood sugar (glucose) in adults with type 2 diabetes mellitus.
According to an analysis from NORC, a research organization at the University of Chicago, nearly half of nearly half of North Carolinians are obese. 45% of the state has a BMI over 30 — a little more than 2% higher than the national average.
Wake County was ranked in the 2023 County Health Rankings report as having the second-best health factors in the state — a measure that factors in obesity. [source]
- Orange County was ranked No. 1, the report, released by the University of Wisconsin Population Health Institute, found.
- Robeson County came in last place.
Read the full FDA press release here.
100,000 NC Residents to Participate in 5 Year Genomics Testing

The hope has always been that genetic testing can lead to better health care and also prevent many health problems in the first place. That hope is going to be put to test in a five-year program in the North Carolina Triad.
Helix, the leading population genomics company in the nation, and Cone Health, a not-for-profit health care network serving people in the North Carolina Piedmont region, will launch a population genomics testing program. It will put precision medicine to work in Alamance, Forsyth, Guilford, Rockingham and Randolph counties and beyond.
The joint project will enroll 100,000 healthy people over a 5-year period. Genetic testing will provide medical insights for Cone Health patients using Helix’s population genomics platform. It is expected that the effort will result in better, more effective care for people who develop health conditions and information that people and their providers can use to potentially delay, reduce or even prevent illness. The program will also help Cone Health uncover what risks might be occurring at disproportionate levels within communities, better understand the health of the overall population and build wellness programs for the broader community.
Enrollment in the program is optional and no cost. Participants will be screened for genetic predisposition for certain diseases and conditions, such as breast and ovarian cancer, colorectal cancer and high cholesterol. Nationwide, nearly five million people are at an increased risk of one of these conditions because of a genetic mutation.
“We’re ready to work together on the positive, life-changing impact this partnership will have on our community members,” says Marlon Priest, MD, Chief Clinical Officer at Cone Health. “This collaborative effort touches everything from our high-quality heart care services to our commitment to health equity across our communities.”
With its end-to-end genomics platform, Helix works with health systems across the nation to identify people at risk for diseases and conditions based on inherited genetic mutations. The Cone Health program will be one of the largest population health efforts in the region, enabling all participants and their health care providers to receive important information about their potential risks today and in the future.
Beyond what’s included in this program, Helix will also provide Cone Health with genetic panels for additional health conditions. Thanks to its unique Sequence Once, Query Often™ model, individual patients can have future genomic tests run without the need for an additional sample. This will give them, and their providers, access to ongoing genomic insights about their health throughout their lifetime.
“Partnering with Cone Health, one of the region’s largest and most comprehensive health networks will provide vital information about whether patients have an increased risk of disease. That impact can reverberate through North Carolina families for future generations,” said James Lu, M.D., Ph.D., Helix’s Chief Executive Officer and Co-Founder. “Cone Health is enabling the future of medicine through this program, helping individuals work with their doctors to take greater control of their health. We are proud to partner with them to positively impact public health across the state.”
Cone Health joins Helix’s fast-growing group of population genomics partners across the United States. These programs have already begun having an impact on patients’ health decisions, and the company is on pace to test millions of Americans in coming years. [source]