The Joint Appropriations Health and Human Services Committee met on February 26, 2019.
Medicaid Transformation Implementation
Department of Health and Human Services Secretary, Mandy Cohen, MD provided the Committee an update on Medicaid Managed Care.
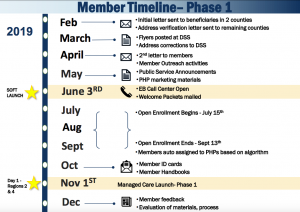
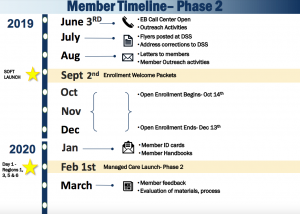
She stated that Regions 2 and 4 will go first iim the process in November of 2019. The remaining Regions will roll out in February 2020. 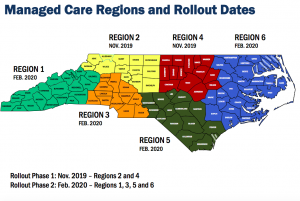
She noted that there has been a protest filed, but they anticipated moving forward with their proposed timeline.
Dave Richard provided an overview on the beneficiary experience. Beneficiaries who don’t choose a health plan automatically based on this criteria:
- Where they live
- If they are a member of a special population (ex. federally recognized tribes BH or I/DD Tailored Plan eligible)
- Plan assignments of other family members
- Beneficiary has a historic relationship with particular PHP
- One time credentialing process instead of credentialing for each process
- Single statewide drug formulary all PHPs are required to utilize
- Same services covered in Medicaid managed care and fee for service
- Department’s definition of “medical necessity” will be used in all PHPs in making coverage decisions
- Providers are offered some contracting “guardrails”