NCMS Staff at Work: Lunch & Learn Webinar: LEGISLATION, EXPECTATIONS & ADVOCACY
https://www.youtube.com/watch?v=j72px9BMNJI
This lunch and learn featured Thomas Kincheloe, NCMS Director of Legislative Affairs, and Alan Skipper, NCMS VP of External Affairs, presenting an overview of the first few weeks of the 2023 legislative long session in NC and a summation of what is happening at the federal level thus far in 2023.
Additional Resources:
On Point: Room with a View - by James E. Hill, Jr., MEd, PA-C Emeritus, DFAAPA
 I have been clinically retired as a practicing PA for several years now after a 42-year career as a PA, mostly in emergency medicine. During that time, a number of patient experiences have remained with me, mostly for the life lessons they taught me. There is one, though, which has haunted me for over 10 years, and I’ve finally decided to banish those demons by sharing the story.
I have been clinically retired as a practicing PA for several years now after a 42-year career as a PA, mostly in emergency medicine. During that time, a number of patient experiences have remained with me, mostly for the life lessons they taught me. There is one, though, which has haunted me for over 10 years, and I’ve finally decided to banish those demons by sharing the story.
In emergency medicine, the practice environment is a closed system. There are no windows and the doors lead to other areas of the ED or the hospital. In wintertime, while working a day shift, it was dark when I left for work and dark when I finished my shift to drive home. The florescent lights on the ceilings are our synthetic sunshine.
One winter’s shift I arrived to discover that the Spanish interpreter we usually used to help us with our Hispanic patients had called in sick, and there was not a backup interpreter available. My first patient was a 12-year-old Hispanic girl who was presenting with 2 weeks of nausea. She spoke English fluently, but her mother did not speak English. I had a dilemma since there were no staff in the ED who spoke Spanish that day.
I decided to speak to the 12 year old since she was intelligent and appeared mature for her age. I did ask her to share my questions with her mother, and her answers with her mother---English to Spanish to English. A history of present illness revealed no associated symptoms---just intermittent nausea throughout the day for 2 weeks. She also told me she had not started having menstrual periods yet and had no boyfriends.
Her physical examination was normal---no signs of dehydration, no icterus, no abdominal discomfort. The decision was then made to obtain some laboratory studies (blood and urine) as a screening assessment. Just before sending these to the lab for analysis, my “6th sense” told me to add a urine pregnancy test. All the labs came back normal except for one---a positive pregnancy test.
I returned to the room to speak to my patient about her lab results. She swore to me, quite adamantly, that the test had to be a mistake as she had no boyfriend and had never had sex. I was determined to uncover the truth, and we continued our discussion for over an hour---her denials and my persistent assertions that it was important to face the truth for her health. Ultimately, she started to cry, then told me that her stepfather had been sexually abusing her for several years, finally progressing to penetration in the past few months. She begged me not to tell her mother, saying that he was the only one who worked in the family and that she, her younger brother and her mother would have no place to live if he was arrested. I convinced her to tell her mother what she had told me. And, I told both of them I had to report this to the police and to the social worker as what the stepfather was doing was harmful to both of them, as well as a crime.
The mother had difficulty accepting the diagnosis and the facts behind the pregnancy. The police arrived as well as a social worker, and the stepfather was arrested in the waiting room. All I could think to say to the 12 year old girl that she would come to realize later this was the only way to heal and move toward a healthy life.
I then returned to seeing other patients after being tied up with one patient for over 2 hours. As is common in emergency medicine, her follow-up was lost to me. At the end of my shift, I drove home in darkness, thinking about this child and the terrible events bringing her to the emergency department, wondering what would happen to her and her pregnancy, wondering if she and her family would survive the betrayal of trust from her step-father and his path through the criminal justice system, wondering if she would grow wiser in the coming years. It was then I had an epiphany. The emergency department may have no windows, but it is truly a room with a view. It allows us to see people in their worst times, caused by events not of their choosing in most cases, and it allows us as PAs to be part of their lives for a sliver of time when dealing with the results of those events. I’m happy to settle for that.
On Point: CMS needs to include measures for social drivers of health
This op-ed was shared on April 29, 2022, on STAT
By Michael Darrouzet, Jennifer Hanscom and Chip Baggett
Yet even with an ongoing pandemic that has painfully brought these issues to the fore, no measures of social drivers of health exist in any federal quality and payment programs, and these factors are still not accounted for in CMS’s “risk adjustment” calculations — how healthy (or sick) a patient is and, therefore, how much their physician should be paid to care for them.
The Physicians Foundation, whose directors are appointed by 21 state and county medical societies, responded to CMS’s annual invitation for new Medicare measures by putting forward the first two SDOH measures ever proposed. These focus on the percentage of patients who are asked about food insecurity, housing instability, inadequate transportation, interpersonal safety, and difficulties paying for electricity and other utilities; and the percentage of patients who are positive for each of these needs. Even though CMS has declared it a priority to “develop and implement measures that reflect social and economic determinants,” these two measures are the only ones related to social drivers of health and are the only patient-level equity measures in this review cycle.
To truly move the needle to improve health outcomes for vulnerable Americans and give physicians the quality measures they want and need, CMS must act now to incorporate these two measures. Last week, CMS took a crucial first step by proposing these measures for the Hospital Inpatient Quality Reporting Program, which sets rules for Medicare payments to hospitals. Next, it will consider the same measures for the Merit-based Incentive Payment System.
Many stakeholders have emphasized the particular importance of the percentage of patients who screen positive for social needs. The rate itself should not be rewarded or penalized, recognizing that it would be influenced by the community in which a practice exists and its patient population. Yet this measure is essential to make visible and address factors that contribute to health disparities and support improvement activities. In addition, this measure would enable CMS to account for patient-level social drivers of health in risk adjustment, providing a more complete picture of the impact of these factors on health care costs, outcomes and disparities.
Both measures are essential to fulfill CMS’s commitment to health equity — articulated in its recently released health equity strategy pillar and its vision for the Centers for Medicare and Medicaid Innovation and its associated health equity initiatives, all of which cite the importance of routinely and in standard ways “collecting self-reported demographic and social-needs data.”
Over time, these measures of social drivers of health can and will be improved with the benefit of the input of physicians and patients across the country and the data generated by these measures. Yet we also recognize that, given the profound challenges that Covid-19 has wreaked on patients, physicians, and the U.S. health care system at large — and the commitment to equity and the reduction in health disparities that CMS and health care institutions across the country have declared — that time is of the essence in enacting these historic measures of social drivers of health.
Michael Darrouzet is the chief executive officer of the Texas Medical Association. Jennifer Lawrence Hanscom is the chief executive officer of the Washington State Medical Association. Chip Baggett is the chief executive officer of the North Carolina Medical Society. All are board members of The Physicians Foundation, a nonprofit seeking to advance the work of practicing physicians and help them facilitate the delivery of high-quality health care to patients.
About the Authors
Michael Darrouzet
@texmed
linkedin.com/in/michael-darrouzet-4632281/
Chip Baggett
@NCMS_EVP_CEO
linkedin.com/in/chip-baggett-9356966/
On Point: Address rising violence in the ER - by Michael Utecht, MD
This op-ed was shared in several publications including the Raleigh News & Observer and the Charlotte Observer on January 27, 2022
 Picture this: You’re a physician, nurse or other hospital staff member working a Friday night shift in a busy emergency department — where tensions often run high. Local law enforcement officers usher in a violent patient. He is placed in a room, evaluated and kept under guard for several hours.
Picture this: You’re a physician, nurse or other hospital staff member working a Friday night shift in a busy emergency department — where tensions often run high. Local law enforcement officers usher in a violent patient. He is placed in a room, evaluated and kept under guard for several hours.
Before it can be determined that the patient can be released back into police custody, he violently assaults a staff member, as well as the police officer guarding him. He grabs the officer’s weapon and threatens everyone around him. Shots ring out. Hospital police use deadly force to subdue the once patient, now assailant, and staff and patients flee.
This very scenario played out Jan. 14 in the Emergency Department at Duke University Medical Center. Violence in emergency departments and other hospital settings is growing at an alarming rate. Not just in large, urban centers but across the spectrum of healthcare facilities. VA hospitals, small rural hospitals and local community hospitals are not immune from such violence.
According to surveys by the American College of Emergency Physicians and the Emergency Nurses Association, almost half of emergency physicians report being physically assaulted at work, while about 70% of emergency nurses report being hit and kicked while on the job. Nearly 7 in 10 emergency physicians say their hospital reported the violent incident, yet only 3% of the hospital administrators pressed charges. So it is no surprise that 80% of emergency physicians say violence in the emergency department impacts patient care. To compound the problem, the COVID-19 pandemic has increased emergency department use by patients with behavioral health and substance abuse issues, pushing already resource-strained departments to the brink. Unfortunately, state and federal legislators have thus far done little to introduce legislation to prevent such violence. Often focused on “punishment” in the aftermath, no current legislation empowers hospitals to take the necessary measures to prevent violence in the first place. Simple measures such as requiring metal detectors at hospital main and emergency department entrances have proven to be effective as a first line of defense.
Sadly, some hospital administrators feel this promotes a negative image to their “clients,” although multiple studies have proven the contrary. Certainly metal detectors do not seem to deter anyone from attending a sporting event! Fortunately, groups like the American College of Emergency Physicians and Emergency Nurses Association continue to advocate for meaningful legislation to address violent crime in hospitals. Only time will tell if their efforts will put an end to the violence. But, quite frankly, time is running out. The frequency of violent attacks on nurses, physicians and patients in our nation’s emergency departments is unconscionable and unacceptable. For medical professionals, being assaulted must no longer be tolerated as “part of the job.” As one of the Duke Emergency Medicine residents said to me shortly after witnessing the events of that recent Friday night: “I never thought I was entering a profession where I could be killed!”
Michael Utecht is an emergency medicine physician in Durham and current president of the N.C. Medical Society.
NCMS Morning Rounds for Oct. 15, 2021
While the NC House and NC Senate have an agreed upon budget document, which has not been made public, negotiations are ongoing with Governor Roy Cooper to finalize a state spending plan. We hear there is an announcement planned for next week, so stay tuned and watch your NCMS Morning Rounds newsletter and next Friday's video for updates.
It's LEAD Health Care Conference time! We hope you enjoyed our NCMS PAC legislative forum last night! There is lots more to come today and tomorrow as our sessions address timely topics of importance to you, your practice and your patients.
NCMS Political Pulse for Oct. 8, 2021
The focus this week at the General Assembly was an energy bill moving through committee while budget negotiations continue between legislators and the Governor. We may see a final spending plan next week, so stay tuned.
Be sure to register for our 2021 Virtual LEAD Health Care Conference, which kicks off next Thursday, Oct. 14, with our NCMS PAC event featuring an all-star line up of legislator panelists to discuss the issues that impact your practice. Learn more and register here.
NCMS Political Pulse for October 1, 2021
Finally, we've reached the last step in the state budgeting process and hope to have a final product by mid-October. The NC House and Senate reached an agreement and are now negotiating with Governor Roy Cooper on a final state spending plan. We will continue to monitor this closely.
Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, discusses the latest legislative news including movement on SB85-- Allow Vision Service Plans, and gives you the list of exciting NCMS events coming up!
NCMS Political Pulse for Sept. 24, 2021
This week, NCMS Director of Legislative Relations Sue Ann Forrest, MPA, welcomes NC Sen. Jim Perry (R-Lenoir) to discuss SB257 -- Medication Cost Transparency Act, which regulates pharmacy benefit managers and recently was signed into law. Sen. Perry also offers a budget update and advice on how to make sure your voice is heard.
NCMS Political Pulse for September 10, 2021
It was a short and relatively uneventful week at the General Assembly this week as budget negotiations continue and we continue to advocate for our NCMS budget priorities. We expect to see a final budget document toward the end of September.
One item of note this week involves a letter to key legislators from Blue Cross and Blue Shield of NC voicing support for SB249/HB277 the SAVE Act. The NCMS opposes this legislation, which would grant independent practice to advance practice nurses. We have re-distributed our SAVE ACT Opposition Letter September 2021 describing our -- and many other specialty and county societies' -- opposition. Be sure to read your NCMS Morning Rounds on Monday for more information on this issue.
NCMS Political Pulse for Aug. 20, 2021
This week budget conferees were named. These individuals, who included committee chairs and democratic House members who had voted in favor of the House budget, will continue their negotiations over a state spending plan in the coming week. A side-by-side comparison of both the House and Senate budgets is available on our NCMS legislative blog.
While the budget process is underway, a number of other bills are still making their way through committees. These include:
- SB257 -- Medication Cost Transparency Act, which seeks to regulate pharmacy benefit managers.
- SB608 -- Dignity for Women Who are Incarcerated. We are working closely with the NC Obstetrical and Gynecological Society on this legislation.
- SB711 - NC Compassionate Care Act, more commonly referred to as the medical marijuana bill, which headed back to the Senate Judiciary Committee for discussion.
- SB228 -- Allow Employers to Offer EPO Benefits. The NCMS spoke against this legislation, which would allow narrow networks, in committee this week. Learn more by watching NCMS Director of Legislative Relations Sue Ann Forrest, MPA, in this week's video.
NCMS Morning Rounds 8-13-21
May this Friday the 13th be lucky!
Enjoy your NCMS Morning Rounds.
August 13, 2021
Get Paid to Counsel Medicaid Patients on COVID Vaccination
To help encourage vaccination to protect against COVID-19, NC Medicaid will pay for counseling a Medicaid beneficiary about receiving the COVID vaccine.
Remember – and use -- Code 99401. This is for preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual, for up to 15 minutes, when you counsel Medicaid beneficiaries regarding the benefits of receiving the COVID-19 vaccine whether the patient chooses to receive the vaccine or not.
Learn more about this in this NC Medicaid Bulletin. For questions, please contact the NCTracks Call Center: 800-688-6696.
Be Prepared – Have Adequate PPE on Hand
As the number of COVID-19 cases are again on the rise, and mask mandates are again being put in place, be sure your supply of personal protective equipment (PPE) is adequate for the coming weeks and months. Suppliers are warning us that with increased lead times due to global capacity constraints and increased demand, we may see shortages in the future. Also, transportation challenges due to container shortages and congestion at US and ports around the world are causing shipment delays of all types.
Last year, thanks to state funding, the NCMS was able to distribute free PPE to practices throughout the state to help replenish depleted supplies and create a stockpile for future use. We also joined with other medical societies through ActionPPE to offer a way to order necessary equipment easily through out website.
Now, we recommend you check out Henry Schein, a medical equipment supplier, to help you be properly prepared. Learn more and order from Henry Schein here.
Resources to Help Comply with New OSHA Standard
The federal Occupational Safety and Health Administration (OSHA) published a COVID Emergency Temporary Standard (ETS) back in June. The standard, which currently is in effect, aims to protect health care and health care support workers from exposure to COVID-19 in setting where people with COVID-19 are reasonably expected to be present. Health care employers must develop and implement a COVID-19 plan to identify and control COVID-19 hazards.
This has generated many questions about how to comply among medical practices. Below are links to some helpful resources.
- Is Your Workplace Covered by the ETS?
• A template for developing an OSHA COVID Compliance Plan, prepared by OSHA, that health care providers can use when developing or assessing their plan for compliance
• OSHA COVID-19 ETS Fact Sheet
• June 25 webinar by OSHA
In the News
See the Data on Breakthrough COVID Hospitalizations and Deaths by State, The New York Times, 8-10-21
Learning Opportunity
Registration for the comprehensive Duke-UNC Tobacco Treatment Specialist Training (TTS) Fall Program, Oct. 25-Nov. 2, is now open. Also, three NEW 1-day intensive CME trainings are available.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for Aug. 6, 2021
HB96--Allow Pharmacists to Administer Injectable Drugs, was heard in the Senate Rules Committee and received a unanimous favorable vote on the Senate floor before being sent back to the House for concurrence. While there were no amendments to the legislation, one requirement remains -- parental consent must be obtained when administering a vaccine with Emergency Use Authorization only to a minor. In other legislative news, the NC House released its budget. Funding for the ECU telepsychiatry program along with additional money for health departments -- both funding provisions we support -- were included. A vote on the House budget is anticipated next week. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, gives you all the week's legislative highlights.
Please note you can always view the latest health care bill summaries and sign up for Action Alerts on our legislative blog: www.ncmedsoc.org/currentsession.
Political Pulse for July 23, 2021
While this week was supposed to be a lighter week at the General Assembly, several health related bills did move. HB96--Allow Pharmacists to Administer Injectable Drugs, was heard in the Senate Health Committee and referred to Senate Rules. The NCMS has been working with a variety of stakeholder groups to modify this bill and has been able to make several positive changes. Review the details of its progression here. Other bills moving this week include HB415 -- Update Chiropractic Laws and SB711 -- NC Compassionate Care Act, which seeks to legalize medical marijuana. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA reviews the week's legislative highlights.
NCMS Morning Rounds 7-22-21
Enjoy Thursday's NCMS Morning Rounds.July 22, 2021Medicaid Managed Care UpdatesJust a reminder that the latest NC Medicaid Bulletin has been issued and contains a variety of updates on issues around Medicaid managed care including non-emergency transportation for NC Medicaid Managed Care and the new prior authorizations required for substance use disorder prescriptions. The Bulletin also notes the deadline extension for completing the Health Equity Payment Survey. Read the latest on these and other Medicaid topics here. The July 2021 Medicaid Pharmacy Newsletter also is now available and includes information on Medicaid managed care transferring prior approvals and pharmacy billing and contracting Information. Access the newsletter here. As you are navigating the new Medicaid managed care landscape be sure to visit our Medicaid Transformation webpage. There you will find resources for each of the pre-paid health plans and links to the state’s information. If you have an issue that can’t be resolved by an individual plan or NC Medicaid, please complete our Medicaid Transformation Issues Form so we can track challenges and work to help address them for our members and their patients. Dr. Tilson Honored by NC Institute of Medicine BoardThe NC Institute of Medicine’s (NCIOM) Board of Directors recently honored fellow NCIOM Board member and State Health Director and Chief Medical Officer Betsey Tilson, MD, MPH for her ‘extraordinary efforts to protect the public’s health and prevent human suffering during the coronavirus pandemic of 2020-2021.’ Board Chair David Sousa, JD, Chief Operating Officer and General Counsel for Curi, presented Dr. Tilson with a plaque and stated the hope that “your great-great grandchildren, who’ve read about this crazy pandemic in their history books, will continue to display this as a testament to the legacy of excellence by you, in their family and in our state.” Sousa expressed gratitude for Dr. Tilson’s tireless work to respond to the pandemic. “There is no perfect pandemic response,” Sousa said in presenting Dr. Tilson with the plaque. “But there is courage, dedication and commitment, and you have shown these qualities and inspired them in others.” Improving Outcomes for Ill, Injured ChildrenThe presence of an individual with an interest in pediatric emergency care has been shown to significantly improve outcomes for ill and injured children. This Pediatric Emergency Care Coordinator Workforce Collaborative seeks to develop any health care professional working in the prehospital or emergency department systems into highly effective champions of pediatric readiness. This collaborative invites interested health care professionals to participate a couple of hours a month to become highly effective champions of pediatric readiness and improve outcomes for ill and injured children. Learn more about how you can become involved and register for this training here. In the NewsMore Than 200 People in US Being Monitored for Possible Monkeypox Exposure, CDC Says, STAT, 7-20-21 Learning OpportunityJoin the NC Medical Group Management Association on Thursday, July 29 at 1 p.m. for a webinar on OSHA ETS Q & A Session with the NC Commissioner of Labor Josh Dobson. This virtual event will address the impact of the OSHA ETS on medical practices. You may submit questions for Commissioner Dobson when you register. Learn more and register here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 7-20-21
Here is your Tuesday NCMS Morning Rounds.
July 20, 2021
Don’t forget today’s Lunch & Learn Webinar -- Health Equity in Context.
Cornell P. Wright, MPA, Executive Director of the NC Department of Health and Human Services Office of Minority Health and Health Disparities is our speaker. Join us from noon to 1 p.m. today. Learn more and register here.
Letter Details Opposition to the SAVE Act
As reported previously, the NCMS along with several specialty societies met with legislators last week to discuss SB249/HB277 -- the SAVE Act, which would remove the current physician supervision requirements for nurse practitioners, certified nurse midwives, clinical nurse specialists and certified registered nurse anesthetists within the definition of advanced practice registered nurse.
NCMS Past President and chair of the NCMS' Medical Team Task Force Robert 'Charlie' Monteiro, MD, spoke at the meeting about the NCMS' opposition to this proposal and about the importance of training and education to patient safety. The NCMS and numerous medical specialty societies sent a letter to legislators outlining our opposition to the SAVE Act. Read the updated letter here.
We need you, NOW, to act, engage, and communicate with your legislators on this issue. Please use the Find Your Legislator link and contact your legislator to discuss the importance of training and education, and why both are crucial to quality patient care.
Don’t Miss this Opportunity to Learn and Grow with Leadership College
The NCMS Foundation’s Kanof Institute for Physician Leadership (KIPL) is now accepting applications for its 2022 class of Leadership College scholars. This highly thought of program offers a comprehensive look at leadership development, bringing together a diversity of colleagues from a wide variety of specialties, practice models and geographic location within NC. Leadership College is unique because it also offers participants access to the NCMS’ special position in the state’s health care community with opportunities for a firsthand look at our advocacy efforts and our many other innovative initiatives.
If you would like to learn more, please submit a Leadership College interest form here or email Aubrey Cuthbertson at [email protected].
Learn more about the Kanof Institute for Physician Leadership and all its programs here.
Power Hour Is Cooling Off for the Summer
The NCMS Foundation’s Power Hour educational sessions are on summer break.
In the meantime, visit our archive of previous Power Hours to learn about some of the hottest topics of the last 18 months. Scroll through our Power Hour library here.
In the News
Treating the Unvaccinated, The New Yorker, 7-16-21
Learning Opportunity
Understanding Potential Menthol Tobacco Bans and their Impact on Communities of Color
Tomorrow, Wednesday July 21 from noon to 1 pm.
On April 29, 2021, the U.S. Food and Drug Administration announced that it would issue proposals within the next year to ban menthol cigarettes and all characterizing flavors in cigars. This session will outline the latest science on nicotine initiation, addiction, and cessation, the use of flavorings in tobacco products, as well as the disparate impact of menthol tobacco products on various populations, especially communities of color.
Expert panelists will also discuss key milestones of tobacco and nicotine-related policies at the state and federal level and outline the opportunities and challenges of implementing the FDA’s forthcoming menthol bans.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for July 16, 2021
This week, the NCMS along with several specialty societies met with legislators to discuss SB249/HB277 -- the SAVE Act, which would remove the current physician supervision requirements for nurse practitioners, certified nurse midwives, clinical nurse specialists and certified registered nurse anesthetists within the definition of “advanced practice registered nurse. NCMS Past President and chair of the NCMS' Medical Team Task Force Robert 'Charlie' Monteiro, MD, spoke at the meeting about the NCMS' opposition to this proposal and about the importance of training and education to patient safety. The NCMS and numerous medical specialty societies sent a letter outlining our opposition to the SAVE Act. Read the letter here. And watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, offers more detail on this meeting and other news from the General Assembly.
NCMS Political Pulse for July 2, 2021
The state's long awaited transformation to Medicaid managed care took place this week To aide in finding the resources and help you may need in this transition, the NCMS, working with our partners, has compiled necessary resources and a form to submit with any issues you encounter during this change. Access the page here. In other legislative action, several bills the NCMS supports including one regulating pharmacy benefits managers and one providing enhanced resources for school nutrition programs moved. Also, SB711- the NC Compassionate Care Act, which deals with medical marijuana unanimously passed the Senate Judiciary Committee this week. Watch as Sue Ann Forrest, MPA, NCMS Director of Legislative Relations, offers more information on the NCMS position on this and other important legislation.
Please note you can always view the latest health care bill summaries and sign up for Action Alerts on our legislative blog: www.ncmedsoc.org/currentsession.
NCMS Morning Rounds 6-11-21
T.G.I.F! Enjoy your NCMS Morning Rounds.
June 11, 2021
Broad Health Care Coalition Supports Medicaid Extension for Postpartum Care
In a press release issued Thursday, June 10, 2021, the North Carolina Medical Society (NCMS) brought together a broad coalition of health care associations (NC Academy of Family Physicians, NC Pediatric Society, NC Obstetrical and Gynecological Association, NC Academy of Physician Assistants, NC Osteopathic Medical Association, NC Chapter of the American College of Physicians), representing thousands of physicians and PAs throughout North Carolina, to publicly declare our support for this important legislation (SB530 – Medicaid for Twelve Months Postpartum) extending Medicaid coverage for new mothers to a full year after the birth of their child. Research has shown that insurance during this critical postpartum period is associated with better outcomes for both mother and child.
“The NCMS has long supported efforts to reduce the rates of maternal mortality in North Carolina as well as policies that seek to improve maternal and infant health,” said NCMS President Philip Brown, Jr., MD. “Health challenges from pregnancy often extend up to a year postpartum, and a lack of insurance coverage is connected with worse outcomes for mothers and infants. The bill currently under consideration addresses this issue and is especially vital for women of color and immigrant women who disproportionately suffer from poor health and high maternal mortality rates.”
The state’s current Medicaid coverage for new mothers leaves roughly half of new mothers uninsured 60 days after delivery of their baby, according to the North Carolina Institute of Medicine’s (NCIOM) 2020 Perinatal Systems of Care Report.
Read full press release here.
White House Virtual Conversation TODAY!
On behalf of the White House COVID-19 Response Team and the U.S. Surgeon General, Primary Care Providers, Health Systems, and State and Local Health Officials are invited to a virtual conversation on Primary Care Providers, Health Systems, and the Next Phase of the Vaccination Rollout. The event is TODAY, Friday, June 11, from 3:00 – 4:00 PM ET.
The event will be an opportunity to thank primary care providers and health systems for their service to their patients, state, and country throughout the COVID-19 response and vaccine rollout. It will focus on the importance of primary care providers and health systems in further expanding efforts to administer vaccination programs and educate their patients on the vaccine, as well as the tools the federal government is providing to support them. It will also touch on how state and local health departments can help enable vaccinations at primary care provider offices.
The event will feature five conversations with primary care providers, health system leaders, and state health officials on innovative approaches they are taking to patient outreach and implementing vaccination program at primary care provider offices. Each conversation will be chaired by a different public health leader from the Biden Administration – Dr. Fauci, Dr. Walensky, Dr. Murthy, Dr. Nunez-Smith, and Dr. Choucair.
Again, join this conversation TODAY, Friday, June 11—3:00-4:00 PM ET.
Please click the following link during the event to attend.
A recording will also be available at this link after the event.
ActionPPE Closeout Sale on Medical Supplies
With the pandemic waning, ActionPPE will soon be ending their online sales. As a final benefit to NCMS members, they’re offering a 30 percent DISCOUNT on items such as control syringes, needles, exam gloves and more!
To access this great offer, visit actionppe.org/ncms, and use code THANKYOU30
Discount expires on June 15, 2021!
It’s A Celebration!
The New Hanover-Pender County Medical Society is having a celebration, and you are invited. The event welcomes fully vaccinated physicians, NHPCMS members, their spouses or guests. See invitation below for details.
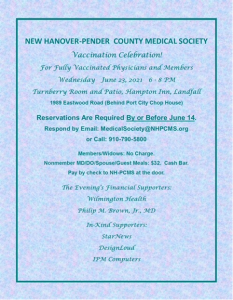
Please RSVP by Monday, June 14, 2021, by sending an email to [email protected] or calling 910-790-5800.
In the News
Why Experts Are So Worried About The 'Delta' Coronavirus Variant, Advisory Board, 6-9-21
Learning Opportunity
Join the Centers for Medicare & Medicaid Services (CMS) for its two upcoming webinars titled CMS Quality Measurement: Where It’s Headed and How We’ll Get There and Driving Quality in the US: How CMS Evaluates its Measure Portfolio. These webinars will illuminate audiences on CMS’s efforts to enhance the quality of quality measures. In the first webinar, CMS will discuss goals for advancing quality measurement in the next 5-10 years, focusing on streamlining measures to reduce burden and the transition to digital quality measures. CMS staff will provide an overview and highlight key components of its newly finalized Digital Quality Measurement Blueprint. The second webinar will walk audiences through CMS tools and processes, specifically the MMS Blueprint, Pre-rulemaking process, Quality Measure Index, and Impact Assessment, to evaluate the quality of its quality measures throughout the measure lifecycle. Both webinars will provide information to key quality measurement resources available to the public. Each webinar will be offered twice this summer:
- CMS Quality Measurement: Where It’s Headed and How We’ll Get There
- Tuesday, June 15, 2021, from 3:00 p.m. – 4:00 p.m., ET (Register here)
- Thursday, June 17, 2021, from 12:00 p.m. – 1:00 p.m., ET (Register here)
- Driving Quality in the US: How CMS Evaluates its Measure Portfolio
- Tuesday, July 13, 2021, from 1:00 p.m. – 2:00 p.m., ET (Register here)
- Wednesday, July 14, 2021, from 3:00 p.m. – 4:00 p.m., ET (Register here)
For questions about the webinar, please contact [email protected].
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 6-10-21
Happy Thursday! Enjoy your NCMS Morning Rounds.
June 10, 2021
Physicians Still The Top Choice For Patients According To National Tracking Poll
Conducted between April 29-May 2, 2021, the Morning Consult’s National Tracking Poll sampled 2,200 adults on health care usage and trust. The interviews were conducted online and the data was weighted to approximate a target sample of adults based on gender, educational attainment, age, race and region. In general, the study found adults were more likely to say they would select a physician’s office over a retail health clinic or an urgent care center for a variety of health care services, though there were significant differences by the age of the respondent.
- 59 percent of adults said they trust their primary care doctor a lot, while 24 percent said they trust the healthcare industry, and only 15 percent said they place a lot of trust in retail health clinics.
- 70 percent of adults would select a physician’s office for wellness checkups, and 67 percent for blood work, while 62 percent would select a physician’s office for diagnosing and treating common illnesses and 56 percent for vaccinations.
- 84 percent of adults said cost of services is somewhat or very important when it comes to retail health clinics.
- There was a significant difference by age of almost 30 percent between adults under 35 and those 65 or older when it came to their preference for getting a wellness visit, treating a common illness, and getting blood work done at a physician’s office. Almost half of adults under 35 said they would go to a physician’s office for this care, while more than four in five adults 65 or older would go to a physician’s office.
Click here to view the full report.
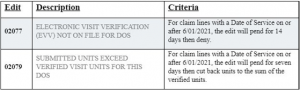
Reminder: Electronic Visit Verification Implementation - Claim Adjudication Based on EVV Data Began June 1, 2021
NC Medicaid ended the pay and report period for Electronic Visit Verification (EVV) claims on May 31, 2021. Claims submitted for Dates of Service June 1, 2021 and after will be required to validate EVV data prior to claims adjudication. There are two edits for EVV that will be applied if the claim submitted does not have the required EVV data. Once applied, these edits will pend for an identified number of days to allow for the issue to be resolved prior to denial of the claim.
For claim lines with a Date of Service on or after 6/01/2021, the edit will pend for seven days then cut back units to the sum of the verified units.
Providers utilizing Sandata, the State’s EVV solution, should ensure that all visits are verified in the EVV portal prior to submitting claims. A visit with the status of verified, means there are no exceptions. Clearing or resolving all exceptions on an incomplete visit updates the visit status to ‘verified.’ Providers utilizing an alternate EVV (Alt EVV) solution may confirm verified visits with their vendor and may also view visits in the Sandata Aggregator.
For more information about EVV, please visit the NC Medicaid EVV webpage.
June is National COVID-19 Vaccine Month of Action
The US Department of Health and Human Services (HHS) “We Can Do This” COVID-19 Community Corps has kicked off a month-long mobilization effort to get our communities vaccinated by July 4th! The National Vaccine Month of Action is a collaborative effort with thousands of national organizations, community-based partners and everyday people, serving as trusted messengers, listening to people’s concerns, and helping them make informed decisions about COVID-19 vaccinations.
There are plenty of ways to take action near you or virtually. You can find more opportunities to participate here.
In the News
CDC: Milder, Shorter Illness For Fully Vaccinated People Who Develop Breakthrough Infections, Becker’s Hospital Review, 6-8-21
Learning Opportunity
Carolina Medical Home Network (CMHN ) Care Management Training, June 14 @ 8 am - June 22 @ noon
Due to COVID-19 and the need to minimize costs, Carolina Medical Home Network (CMHN) will be offering an initial Care Management training in multiple half-day sessions June 14, 2021-June 22, 2021 from 8am-12pm. The training team will incorporate approaches that encourage hands-on learning and application of material where applicable in this virtual environment.
To support targeted learning, breakout sessions will be offered to tailor the content for the roles of care manager and care coordinator.
The richness of the content will ensure all care managers and care coordinators are fully prepared to succeed in the landscape of Managed Medicaid. Attendees will administer a pre and post assessment to evaluate their competency for each subject covered during this training.
There is a cost of $275 for the training and participation is mandatory for Care Managers and Care Coordinators within the first six months of go-live.
Click here for more information and to get tickets.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 6-7-21
Here's your Monday NCMS Morning Rounds.
June 7, 2021
NCMS Legislative Update
Last week was a busy one at the General Assembly. The budget process has started. However, the House and the Senate have been unable to reach an agreement on a spending amount, both in recurring and non-recurring dollars. The House decided to move forward with their own process, having each individual appropriations committee to meet to discuss their priorities. The Health Appropriations Committee on the House side met to discuss some legislators’ top priorities. There will be a lot to come in upcoming weeks on budget updates, so stay tuned.
While a lot of Senate dialogue was spent on confirmation of the Governor’s pick for secretary of the NC Department of Environmental Quality last week, several bills moved through the process, including SB257 -- Medication Cost Transparency Act. There was an amendment in the Senate, so this bill will go back to the House. We will continue to update you on this bill’s progress.
HB453 -- Human Life Nondiscrimination Act/No Eugenics moved through two Senate committees. We expect it to move through Rules and the Senate floor, likely, this week. The NCMS believes this bill interferes with the physician-patient relationship and we stand with the North Carolina Obstetrical & Gynecological Society (NCOGS) in opposing this bill.
HB224 -- Occupational Therapy Interstate Compact is currently sitting on the Governor’s desk. We’ll update you when—or if—the Governor signs this bill.
SB116 -- Putting North Carolina Back to Work Act has received a lot of attention from the media and garnered discussion on the House side. It passed the House late on Thursday and has been sent back to the Senate for concurrence. More to come on this bill.
It’s likely to be a budget-filled week this week. Stay tuned for updates.
Are You Up to Speed?
The North Carolina Broadband Survey is designed to gather information on locations in the state without adequate internet access and speeds.
The information gathered from the survey will:
• Provide clear data to guide investment of funds through the state’s Growing Rural Economies with Access to Technology grant program
• Inform research and policy recommendations
• Support strategic targeting of additional funding streams
The survey is a collaboration between the N.C. Department of Information Technology’s Broadband Infrastructure Office and the Friday Institute for Education Innovation at NC State University.
The survey takes about 5 minutes to complete and is available in both English and Spanish. Participants are encouraged to also take the optional internet speed test to connect survey data with broadband speed information.
Prior Approval Requirement for High Tech Imaging Terminating July 1, 2021
Effective for dates of service on or after July 1, 2021, prior approval (PA) for high tech imaging services (ultrasounds, computed tomography [CT], magnetic resonance [MRI] and positron emission tomography [PET]) will no longer be required for North Carolina Medicaid fee for service (Medicaid Direct) beneficiaries.
Beginning July 1, 2021, providers who contact eviCore will be notified that a beneficiary either does not require PA thorough Medicaid Direct or will be referred to the beneficiary’s prepaid health plan for assistance. PA is still required for high tech imaging services for delegated beneficiaries for dates of service prior to July 1, 2021. Retroactive eligibility will continue to be managed by eviCore.
NC Medicaid is in the process of end dating clinical coverage policy 1K-7, Prior Approval for Imaging Service that will be effective July 1, 2021.
To assist with this transition, NC Medicaid requests that imaging claims with dates of service prior to July 1, 2021, be submitted by Sept. 30, 2021.
In the News
A pandemic upside: The flu virus became less diverse, simplifying the task of making flu shots, STAT, 6-2-21
Learning Opportunity
Hot Topics with Health Plan Chief Medical Officers, Thursday, June 17 | 5:30-6:30 PM
Hosted by Shannon Dowler, MD, Chief Medical Officer of the NC Division of Health Benefits, the Medicaid Managed Care webinars on the 1st and 3rd Thursday of the month are dedicated to bringing you late breaking information and guidance on NC Medicaid’s transition to Managed Care.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for June 4, 2021
The budget process is underway -- sort of -- at the NC General Assembly. Neither the House nor Senate could agree on a spending amount, so each chamber's appropriations committees are meeting to discuss spending priorities. This will likely continue into next week and beyond as legislators work through a budget for the biennium. Some other legislative proposals did continue to move. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, describes those bills. Keep up with all the daily activity at the NC General Assembly at the NCMS legislative blog here.
NCMS Morning Rounds 6-4-21
Happy Friday! Here's your NCMS Morning Rounds.June 4, 2021Please Share Your Experience! Don’t forget TODAY’s Power Hour: Health Equity in Palliative and End-of-Life CareThe pandemic dramatically highlighted the depth of health disparities in our country, but illness and death rates are not the only sources of health inequity in this country. There are also substantial differences in the care that patients with serious illnesses receive near the end-of-life that are based on race or socioeconomic status. Please join your colleagues for this week’s Kanof Institute for Physician Leadership (KIPL) Power Hour, today, June 4 at noon, when our discussion will focus on health equity as it relates to palliative and end-of-life care. Our guests will offer their insights on striving to achieve equal access to palliative and end-of-life care, addressing each patient’s unique psychological, social and spiritual needs as well as pain and symptom management. Health equity issues impact each of these areas and we invite you to explore them with us. Vax Up or Mask UpNCDHHS has launched a new public campaign encouraging North Carolinians to "Vax Up or Mask Up” to support the new guidance that lifts many of the state’s COVID-19 restrictions. The campaign provides downloadable flyers and social media graphics in both English and Spanish to help transition from the 3 Ws messaging (Wear, Wait and Wash) to the new "Vax Up or Mask Up" campaign. Materials are available for download in the COVID-19 Communications Toolkit. Increasing Equitable Vaccine DistributionA new tool created by NCDHHS that maps social vulnerability and vaccination rates by census tract has helped North Carolina vaccine providers increase vaccinations by 50 percent in 89 underserved communities. “This mapping tool is another great example of how we and our providers continue to rely on data to drive our work and help every North Carolinian have easy and convenient access to a COVID-19 vaccine,” said NCDHHS Secretary Mandy K. Cohen, MD, MPH. The department has focused on 90 census tracts identified as having high social vulnerability, low vaccination rates and no COVID-19 vaccine providers as of April 24. Of these 90 census tracts, 89 have achieved a 50 percent increase in vaccinations since April 24 with the state’s targeted outreach efforts. The NCDHHS census tract COVID-19 map is updated weekly. For more North Carolina vaccination data, visit the state's vaccination dashboard. In the NewsChanging the equation: Researchers remove race from a calculator for childbirth, STAT, 6-3-21 Learning Opportunity2021 Society for Advanced Bronchoscopy (SAB) Summit – Virtual, June 12, 2021, 7:30 AM - 3 PM This annual summit will provide updates in advanced bronchoscopy and pulmonary medicine topics provided by a diverse group of physicians to an audience of fellow physicians, advanced practice providers, nurses and respiratory therapists. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 6-1-21
Enjoy your first NCMS Morning Rounds of June.June 1, 2021NCMS Legislative UpdateThis week at the NC General Assembly several bills of note for physicians and PAs were moving quickly including HB395 -- Extend Deadlines for Mandatory HIE Participation, which would extend the deadline for connection to the state's Health Information Exchange (NC HealthConnex) for certain groups, including psychiatrists. This legislation passed through both chambers and currently is on the Governor's desk awaiting his signature. Thank you to everyone who responded to our survey on whether your practice is connected to the HIE. Your input provided crucial information as legislators considered this bill and gave NCMS staff insights into your challenges and how we can develop resources to respond. Other legislative proposals being heard include SB257 – Medication Cost Transparency Act, which sets out criteria for regulation of pharmacy benefit managers. The NCMS supports this proposal, which is moving quickly through the process and will likely pass both chambers. HB947 – The GREAT Broadband Expansion Act, which we believe is indeed a ‘great’ bill providing strong financial investment in ensuring broadband access in rural and underserved communities, is swiftly making its way through the House and we are hopeful the senate will also move quickly to provide this funding. The NCMS has long been supportive of the GREAT grant program as it would expand broadband and enhance access to telehealth, education and job opportunities. While legislators are busy considering a wide variety of bills, there is still no budget proposal. Usually at this point in a long legislative session spending proposals have been presented and negotiations are underway. This delay in the budget process means the session will likely continue for quite a while. It also presents you a great opportunity to contact your legislators to discuss your biggest concerns and where you’d like to see funds allocated. If you don’t already have your legislator’s information for ready access in your contacts, here is where you can easily find it. Breakdown of Medicaid EnrolleesAs the July 1 ‘go live’ date for the state’s transition to Medicaid managed care approaches, the NC Department of Health and Human Services (NCDHHS) recently released the total number of Medicaid enrollees in each of the five pre-paid health plans that will be providing Medicaid services. For those beneficiaries who did not select a plan during the open enrollment period, which ended May 21, the state auto-assigned them using a process (outlined here) in which existing relationships with a primary care provider were prioritized. The state said that 97 percent of those eligible were enrolled in a plan that includes their current PCP in network. Read the state’s announcement here. The breakdown of enrollees in each plan is as follows: Urban Institute Equity ScholarsIn recent months, the Urban Institute has escalated its efforts to provide timely, evidence-based, research and analysis to inform policy and advance racial equity. Towards this goal, Urban is launching its Equity Scholars program offering emerging and established scholars the opportunity to deepen their own research on race, equity, and/or structural racism while contributing to equity-focused analyses underway at Urban. Application deadline is TODAY: June 1, 2021 In the NewsA New Tool Tracks Health Disparities In The U.S. — and Highlights Major Data Gaps, STAT, 5-26-21 Learning OpportunityMIPS Improvement Activities and Promoting Interoperability Performance Categories for the 2021 Performance Year, Wednesday, June 9 from 1 – 2:30 p.m. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Political Pulse for May 28, 2021
This week at the NC General Assembly several bills of note to physicians and PAs were moving quickly including HB395 -- Extend Deadlines for Mandatory HIE Participation, which passed through both chambers and currently is on the Governor's desk awaiting his signature. While legislative proposals are being heard, there is still no budget proposal, which is usually being negotiated at this point in the legislative session. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, fills you in on what this may mean for you.
NCMS Morning Rounds 5-27-21
Enjoy your Thursday NCMS Morning Rounds.
May 27, 2021
If you have not yet completed our 4-question survey on the NC Health Information Exchange (NCHIE) your input will help our advocacy on your behalf. Take the survey now. We also invite you to send us any questions you might have about connecting to the NCHIE. Simply reply to this email with your question and NCMS staff will work to get it answered. Thank you for engaging with us on this topic!
NCMS, NCPeds and Family Physicians Encourage COVID-19 Vaccine for Teens
Yesterday the NCMS, NC Pediatric Society and the NC Academy of Family Physicians sent a joint press release to statewide media urging families to get their teenagers vaccinated against COVID-19. Read the release here.
“As we have said since the first COVID-19 vaccine was authorized early this year, everyone who is eligible should get vaccinated. It is the most immediate and effective way to stop this pandemic,” said NCMS President Philip Brown, Jr., MD, in the release.
Currently, the Pfizer vaccine can be given to teenagers ages 12 and up. The North Carolina Department of Health and Human Services (NCDHHS) reports in North Carolina more than 100,000 children 0 to 17 years old have tested positive for COVID-19 and the percent of COVID-19 cases in children 17 and under has been increasing.
Earlier this week Moderna said its COVID-19 vaccine strongly protects kids as young as 12 in its clinical trials, which will likely put it on track to become the second option for that age group in the U.S. The vaccine producers also are in the midst of clinical trials with younger children.
Podcast on Role of Doulas in Supporting Women with Substance Use Disorders
The Association of Maternal and Child Health Programs (AMCHP) and the National Association of County and City Health Officials (NACCHO) recently released an informative podcast discussing the use of doulas in supporting women in recovery and treatment for substance use disorders.
Two doula certified peer recovery specialists from the Illinois Pregnant and Postpartum Women with Opioid Use Disorder Program, Melinda McMichael, and Joyce Miller, share their experience working at the intersection of substance use care and birthing support. Amy Chen, Senior Staff Attorney of the National Health Law Program’s Doula Medicaid Project and Jessica Stieger, AMCHP Program Manager for Infant Health and Certified Doula, also discuss the role of Medicaid, state public health and opportunities to promote doula care for people with substance use disorders.
Listen to the full podcast here.
Mark Your Calendar for the NCDA’s Summer Meeting, July 9-11
The NC Dermatology Association (NCDA) will host its 2021 Summer Meeting at the Omni Grove Park Inn in Asheville on July 9-11.
The program features outstanding faculty who will address current topics of interest to the practicing dermatologist. The meeting includes a networking hub with vendors presenting products and services to help your dermatology practice. Learn more about the program here.
In the News
CDC releases Breakthrough Infections report: 5 Notes, Becker’s Review, 5-25-21
Learning Opportunity
The Centers for Medicare & Medicaid Services (CMS) is pleased to invite the public to attend its two upcoming webinars titled CMS Quality Measurement: Where It’s Headed and How We’ll Get There and Driving Quality in the US: How CMS Evaluates its Measure Portfolio. These webinars will illuminate the CMS’s efforts to enhance the quality of quality measures.
In the first webinar, CMS will discuss goals for advancing quality measurement in the next 5-10 years, focusing on streamlining measures to reduce burden and the transition to digital quality measures. CMS staff will provide an overview and highlight key components of its newly finalized Digital Quality Measurement Blueprint.
CMS Quality Measurement: Where It’s Headed and How We’ll Get There
o Tuesday, June 15 from 3 – 4 p.m. (Register here)
o Thursday, June 17 from noon – 1p.m. (Register here)
The second webinar will walk audiences through CMS tools and processes, specifically the MMS Blueprint, Pre-rulemaking process, Quality Measure Index, and Impact Assessment, to evaluate the quality of its quality measures throughout the measure lifecycle.
Driving Quality in the US: How CMS Evaluates its Measure Portfolio
o Tuesday, July 13 from 1 – 2 p.m.(Register here)
o Wednesday, July 14 from 3 – 4 p.m. (Register here)
Both webinars will provide information to key quality measurement resources available to the public. Each webinar will be offered twice this summer:
Please register in advance if you can attend, as space will be limited. We request that you please only register for an event if you plan to attend.
For questions about the webinar, please contact [email protected].
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 5-26-21
Happy Wednesday! Here's your NCMS Morning Rounds.May 26, 2021NC Medicaid Transition ResourcesAs the July 1 ‘go live’ date for Medicaid managed care nears, the state is offering a variety of resources to help in the transition. Access the Frequently Asked Questions documents on each topic noted below. Also, the NCMS with the help of other health care organizations are creating a clearinghouse of resources and tips as well as a process in which we will collect input on any issues practices throughout the state encounter as we make this transition. We will use these reports in our conversations with the various health plans and the state to help ensure the challenges are addressed. Watch your NCMS Morning Rounds and your email box for details on this process as the July 1 date approaches. • What Providers Need to Know After Managed Care Launch For more information about NC Medicaid Managed Care, visit the Medicaid Transformation website or the NC Medicaid Enrollment Broker website. Reports of Myocarditis Occurring After COVID-19 VaccinationIn recent weeks, there have been rare reports of myocarditis occurring after COVID-19 vaccination with Moderna or Pfizer vaccines in the United States and Europe. The Centers for Disease Control and Prevention (CDC) is aware of these reports and has been closely monitoring myocarditis/pericarditis in multiple safety systems and will continue to evaluate reports of myocarditis/pericarditis occurring after COVID-19 vaccination and will share more information as it becomes available. The CDC is advising clinicians to be on the lookout for early signs of myocarditis. Read the report here. Myocarditis is the inflammation of the heart muscle and pericarditis is the inflammation of the lining outside the heart. In both cases, the body's immune system is causing inflammation in response to an infection or some other trigger. While myocarditis can be serious, it is frequently mild and self-limited. Symptoms can include abnormal heart rhythms, shortness of breath, or chest pain. Both myocarditis and pericarditis have been reported as complications in patients with COVID-19. While these reports are being further investigated, you should do the following: The CDC continues to recommend COVID-19 vaccination for people 12 years and older. We Need Your Input on COVID-19 Vaccination in Your PracticePlease take just a minute to complete our ongoing survey of how the COVID-19 pandemic is impacting your practice. This week’s survey leads off with questions about COVID-19 vaccination. Your input is invaluable in guiding the NCMS’, the NC Medical Group Management Association’s and Curi’s advocacy on your behalf as well as developing resources to help you over the course of the pandemic. Thank you for your continued engagement! In the NewsCDC says vaccinated people can largely skip testing, shares new breakthrough case count, Becker’s Hospital Review, 5-21-21 Learning OpportunityThe Future of Behavioral Health After A Year of Isolation, Thursday, June 3 • 3-4 p.m. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Political Pulse for May 21, 2021
While the NC House was relatively quiet this week, the NC Senate was busy with several legislative proposals including one bill, HB 395 – HIE Deadline Extension and Patient Protection, which would extend the deadline for connection to the state's Health Information Exchange (NC HealthConnex) for certain groups. To help inform the discussion, the NCMS circulated a survey asking you for input on your experience in connecting to the HIE. Thank you to those who have already responded. If you haven't yet weighed in, please do so here. The survey is only four questions long and your answers will be helpful as we advocate on your behalf on this issue.
Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, fills you in on other bills that are under consideration. And be sure to visit our legislative blog for summaries of all the bills we're tracking.
NCMS Morning Rounds 5-21-21
It's finally Friday! Enjoy your NCMS Morning Rounds.May 21, 2021Don’t forget to take just a minute to answer four questions about the NC Health Information Exchange in this survey. Your input will help our advocacy on your behalf. Take the survey now. Data Shows Many Have Foregone Preventive, Primary and Mental Health CareThe Centers for Medicare & Medicaid Services (CMS) recently released data highlighting the continued impact the COVID-19 pandemic is having on Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries and utilization of health services. The data show that, from March through October 2020, beneficiaries have foregone millions of primary, preventive and mental health care visits due to the pandemic, compared to the same time period in 2019. Although utilization rates for some treatments have rebounded to pre-pandemic levels, mental health services show the slowest rebound. This decline in utilization is occurring at a time when preliminary evidence shows mental health conditions have worsened nationwide, which may have a substantial impact on long-term health outcomes. Medicaid and CHIP-funded mental health services, in addition to primary and preventative services, cover the majority of children, people living in poverty, those with special health care needs and many who are among racial and ethnic minorities. To help close this gap in services, CMS is emphasizing mental health care in its recently launched Connecting Kids to Coverage National Campaign, a national outreach and enrollment initiative funded under the Children's Health Insurance Program Reauthorization Act (CHIPRA) and the Affordable Care Act, that reaches out to families with children and teens eligible for Medicaid and CHIP. Specifically, the data reveals a 34 percent decline in the number of mental health services utilized by children under age 19, compared to the same time period in 2019, and 22 percent decline in the number of mental health services utilized by adults aged 19 to 64, compared to the same time period in 2019. The data does show utilization rates for certain primary and preventive services for children under age 19 have recovered to pre-pandemic levels, or have started to rebound across many areas of the country. While this recovery is encouraging, millions of services still need to be delivered to make up for those missed between March and October 2020. Preliminary 2020 data shows 9 percent fewer childhood vaccinations for beneficiaries under age two (1.8 million services), 21 percent fewer child screening services (4.6 million services) among children under age 19, and 39 percent fewer dental services (11.4 million services) among children under age 19 when compared to pre-pandemic levels. This data takes into account increases in telehealth utilization of services via telehealth, which has shown a marked increase in the number of services delivered via telehealth surging 2,700 percent during the COVID-19 pandemic over previous years. Review the data here. A fact sheet on the Medicaid & CHIP and the COVID-19 Public Health Emergency is available here. RADx-UP CDCC Community Collaboration Mini-Grants AvailableThe RADx-UP CDCC Community Collaboration Mini-Grant Program is open to community serving organizations, faith-based organizations and tribal nations and organizations to help advance capacity, training, support and community experience with COVID-19 testing initiatives. Many communities across the United States are facing more difficulties than others as they confront the COVID-19 pandemic. RADx-UP is working to help those communities most impacted by COVID-19 across the nation. RADx-UP is researching COVID-19 testing patterns and data on disparities in infection rates, disease progression and outcomes and developing strategies to reduce disparities in COVID-19 testing by supporting projects across the country with established community partnerships. The RADx-UP Coordination and Data Collection Center (CDCC) is led by the Duke Clinical Research and the Center for Health Equity Research at UNC-Chapel Hill. Learn more about RADx-UP here. Read more about the RADx-UP CDCC Community Collaboration Mini-Grant Program here. NCMS Book Club Begins The Beauty in Breaking Next WeekThe NCMS Book Club will begin reading The Beauty in Breaking: A Memoir by Michele Harper next Thursday, May 27. If you have not yet joined this online forum of colleagues interested in discussing interesting literature and ideas, please sign up today at this link. A few top reasons why we think you’ll want to grab a copy of this selection and join us in the discussion include: • Michele Harper, MD, is a female, African-American emergency room physician in an overwhelmingly white male profession. Her unique perspective on the challenges facing both healthcare and our nation is thought-provoking and fascinating. We look forward to sharing in the spirited and insightful conversation between you and fellow book club members in our online community as we read The Beauty in Breaking together. These conversations are at the heart of what makes our book club such an enjoyable group! In the NewsIs it safe to 'mix and match' Covid-19 vaccines? Here's what early research shows, Advisory Board, 5-18-21 Learning OpportunityStigma of Addiction Summit, June 10 from noon to 6 pm If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 5-19-21
Here is your Wednesday NCMS Morning Rounds.May 19, 2021Join us at noon this Friday, May 21, for the Kanof Institute for Physician Leadership’s Power Hour when we will host a discussion focused on mental health and indigenous populations. In 2019, nearly 20 percent of Native American adults experienced mental illness and the suicide rate among American Indians and Alaska Native youth is 2.5 times higher than the rest of the US. Learn the facts about mental health issues among indigenous populations, the possible causes and what can be done to eliminate the health disparities that exist. Learn more about this virtual forum and register here. Map Helps Practices with Vaccine Outreach EffortsThe NC Department of Health and Human Services (NCDHHS) has shared a new interactive map based on census tract data the shows the highest rates of social vulnerability (red areas) and the lowest rates of COVID-19 vaccination (smallest turquoise circles. The map also includes the ability to see where COVID-19 vaccine providers and community-based organizations that have offered to support vaccine events are located. This information is useful to help focus the efforts to get as many North Carolinians vaccinated against COVID-19 as quickly and as fairly as possible. The map can also be accessed from YourSpotYourShot.nc.gov. If you have questions, please reach out to [email protected]. In other vaccine-related news, NCDHHS Secretary Mandy Cohen, MD, MPH and pediatrician Kenya McNeal-Trice, MD, will discuss vaccinating adolescents ages 12-15, tomorrow, Thursday, May 20 at 5:30 p.m. Learn more and register for this virtual discussion here. NCDHHS also has information for you, your teen-aged patients and their parents at this link as well as social media posts to help you get the word out to your patients about getting vaccinated. Access the social media toolkit here. Victimized Provider ProjectEach year, Medicare providers have their identities stolen and used to bill Medicare for services, diagnostic tests, or medical equipment that was never provided or not medically necessary. When persons or entities inappropriately bill Medicare and receive payment using a provider’s stolen identity, the legitimate physician or provider may be held liable for any overpayments. CMS’ Center for Program Integrity (CPI) works with providers who claim to be victims of identity theft, and who have suffered financial liabilities in the form of Medicare overpayments or debts, through the Victimized Provider Project (VPP). This program attempts to validate and remediate a provider’s claims as an identity theft victim. Learn how to spot signs of identity theft and protect yourself here. In the NewsCan Covid-19 Vaccines Stop The 'Double Mutant' Variant? Here's What Early Research Shows, Advisory Board, 5-17-241 Learning OpportunitySpecialized Therapies, Optical and Hearing Services, THURSDAY, MAY 20 | 5:30-6:30 PM • Optical & Hearing Services Follow Up If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 5-17-21
Welcome to a new week of NCMS Morning Rounds.
May 17, 2021
NCMS Legislative Update
Last week at the NC General Assembly nearly 100 bills quickly moved through committees and 45 were voted on in either the House or Senate in advance of Thursday’s crossover deadline. While all proposals technically are ‘alive’ until the session officially ends, crossover marks the completion of the first stage of the General Assembly’s work for this long session with the winnowing out those bills with the support necessary to pass through at least one chamber. With crossover behind them, legislators in the House and Senate now will shift their focus to the state budget process, and hope to have a spending plan in place for the start of the state’s new fiscal year on July 1.
While you can see the many bills we are monitoring on our legislative blog here, several among those that remain active after the crossover deadline deserve special mention.
HB96 – Allow Pharmacists to Administer Injectable Drugs which would have allowed pharmacists unrestricted authority to administer any type of injectable. Working with our medical specialty society partners, the NCMS was able to narrow the scope of the language in the proposal to allow only injections pursuant to a prescription, only in individuals over age 18 and mandates reporting back to the prescriber. These changes make the proposal better and safer for patients. We will continue to monitor this legislation so watch your NCMS Morning Rounds newsletter and NCMS Political Pulse video in the coming days for updates.
The other bill of note, SB575 – Pharmacists Improve Public Health Needs, made it through the Senate chamber, but only after the NCMS and our partner medical specialty societies were able to narrow the list of drugs pharmacists would be allowed to prescribe to four – contraceptives, smoking cessation, PEP and pre-natal vitamins. The NCMS and our medical specialty society partners are continuing to work with bill sponsors on the language in this proposal. Watch this newsletter for updates.
As legislators turn their attention to the state budget, now is a great time to reach out to your legislator to discuss not only pending legislation like the bills mentioned above, but also policy priorities to include in the state’s spending plan. If you don’t already have a relationship with your representatives, here is where you can look up how to contact them to begin the conversation about what is important to you as a physician or PA constituent.
Three Ways to Learn About the NC Medical Board's Year
Information about the NC Medical Board’s Annual Report, which gives a comprehensive overview of the Board’s activities for 2020, is available in three formats – in its customary electronic version of the written report, in a short, 2-minute video and also in a podcast.
The report includes licensee demographics, licensing and enforcement data and highlights of NCMB’s work throughout the most recent calendar year.
Access the electronic version here; watch the video here and listen to the 21-minute podcast here.
NCMS Leadership Development Programs Recruiting Now
The NCMS Foundation’s Kanof Institute for Physician Leadership currently is recruiting for two of its programs – Leadership College and Health Care Leadership and Management. Both programs are project-based and focus on developing authentic leadership. That means alumni of the programs have looked inward to examine their own strengths and weaknesses as leaders to understand how to be most effective in driving positive change as part of the larger health care team as well as in the broader community.
The Institute’s Leadership College delves into an individual’s leadership development. Each participant works on a year-long project involving a real-world issue where they can demonstrate their newly acquired leadership insights. At the culmination of the program each scholar summarizes their research findings in a TEDTalk-style presentation we call MEDTalks. You can watch the wide variety of previous years’ presentations here.
Learn more about and apply for Leadership College here.
The Health Care Leadership and Management track has a finance and management component as well as leadership development focus. This year-long course places special emphasis on deeper leadership development and skills that include strategic planning, negotiation and financial literacy and application.
Learn more about and apply for Health Care Leadership and Management here.
Both programs boast small class sizes with lots of personal attention and interaction with faculty and colleagues. The courses went virtual during the pandemic but are now moving toward a hybrid of virtual and in-person sessions.
Interested in hearing from alumni about their Kanof Institute experiences? The Summer 2020 issue of the NCMS Bulletin online magazine features a variety of Kanof Institute alumni recounting their ‘leadership journeys,’ and how the programs helped them each define what leadership means to them and how they currently are using the skills they gained. Read these profiles here.
If you have any questions about the programs, please contact Aubrey Cuthbertson [email protected].
In the News
CDC Backtracks Saying Fully Vaccinated People Can Go Maskless Indoors, STAT, 5-13-21
Learning Opportunity
The NC Department of Health and Human Services (NCDHHS) Immunization Branch invites you to attend a live training session on Tuesday, May 18 from 6 to 7 pm on ‘Becoming a COVID-19 Vaccine Provider: We Need YOU!’ Register here.
This training will help primary care practices understand the Centers for Disease Control and Prevention’s (CDC) COVID-19 Vaccination Program and show how to enroll in North Carolina’s COVID-19 Vaccine Management System (CVMS). CVMS is a secure, cloud-based vaccine management solution for COVID-19 that enables vaccine management and data sharing across providers, hospitals, agencies and local, state and federal governments on one common platform. For more information, please visit the NCDHHS CVMS website here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for May 14, 2021
We are through crossover week at the NC General Assembly and on to the budget process in the coming week. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA explains what's next as well as several important pieces of legislation that moved through the House and Senate chambers and will continue to be considered as the long session progresses.
https://youtu.be/y0BBUUNnVm0
NCMS Morning Rounds 5-14-21
Happy Friday! Here's your NCMS Morning Rounds.
May 14, 2021
Has Your Practice Returned to Pre-COVID Office Procedures?
This week our regular survey includes questions on whether procedures implemented during the pandemic such as checking patient temperatures and social distancing in waiting areas have changed recently. Please take just a moment to complete this survey to help track the evolving impact the pandemic has had on your practice.
Since March 2020, the NCMS, the NC Medical Group Management Association and Curi have been collecting data from these regular surveys to help us advocate on your behalf with policymakers and to develop resources you can use. Thanks to your participation we have a clearer understanding of how North Carolina medical practices have responded to the pandemic and the challenges you face. Thank you!
Position Available on NC Respiratory Care Board
The NCMS has the opportunity to fill a position on the NC Respiratory Care Board. The Board licenses respiratory care practitioners and ensures the qualifications and activities of those engaged in respiratory care are in accord with law and in the best interest of the public. The Board shall issue and enforce standards for the licensure of respiratory care practitioners, but the Board is not a Board of arbitration and has no jurisdiction to settle disputes between private parties. Learn more about the Board here.
Here is some of what would be expected of you as an appointee to the Board:
- Quarterly Board Meetings: Second Thursday of July, October, January, and April
- Quarterly Board Committee Meetings: First Friday of September, December, March, and June
- Members are assigned at least one committee per the Board Chair. The expectation is that they participate in Board Meetings to fulfill 21 NCAC 61 .0101.
The contact for the NC Respiratory Board is its Executive Director William L. Croft, Ed.D, Ph.D., RRT, RCP, who may be reached at (919) 878-5595.
If you are interested in serving on the Board, please contact Evan Simmons at the NCMS, [email protected] by May 18.
NC Medicaid Updates – Today is an Important Day
Today, Friday, May 14, is the last day of open enrollment for Medicaid Managed Care when Medicaid beneficiaries can pro-actively select a pre-paid health plan (PHP) and primary care provider (PCP). This one-pager can help your patients with this process. The fact sheet is available in Spanish here. Those who do not actively select a health plan or primary care provider by the deadline will be auto-assigned.
Today also is the deadline to attest for a June payment as an Advanced Medical Home (AMH) Tier 3 practice. Those who have successfully attested to meeting Glidepath payment eligibility in NCTracks in the previous cycle do not need to do so again.
The NC Department of Health and Human Services (NCDHHS) has developed a reconsideration process following the validation of the provider submitted attestation information. You have the option of requesting an AMH Glidepath Payment reconsideration under the following circumstances:
*You missed the attestation deadline due to hardships related to the COVID-19 pandemic, or
*You disagree with the outcome of the validation determination.
The deadline for submission of Reconsideration Requests is May 23.
For more information, please see the Medicaid bulletin article 'Advanced Medical Home Tier 3 Glidepath Attestation Payment Updates.'
For more information about the transition to NC Medicaid Managed Care, visit the Medicaid Transformation website or the NC Medicaid Enrollment Broker website.
In the News
As America 'Turn[s] The Corner' Against Covid-19, When Will Social Distancing Guidelines Change? Advisory Board, 5-10-21
Learning Opportunity
NC Asthma Summit 2021 – Reimagining Asthma Care in a Digital World, Wednesday, May 19 from 9 a.m. – 1 p.m.
May is National Asthma and Allergy Awareness Month – join with colleagues to learn more during this live morning webinar. Hot topics include COVID-19 & Asthma. Telehealth, ACES & Asthma and new/updated asthma guidelines.
The NC Asthma Summit is a collaboration between the Asthma Alliance of North Carolina (AANC) and UNC Health Sciences at MAHEC.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 5-6-21
Enjoy your Thursday NCMS Morning Rounds.
May 6, 2021
NCMS Issues Joint Statement to Encourage COVID-19 Vaccination
Yesterday the NCMS and the NC Academy of Family Physicians issued a joint media statement urging all eligible North Carolinians to get vaccinated against COVID-19. Now that more medical practices are receiving vaccine supplies, patients have yet another way to access the vaccine in a familiar environment where they can have their questions answered by their trusted physician or PA. Read the statement here.
If you have questions or would like to participate in the vaccination effort, the NC Department of Health and Human Services (NCDHHS) has this ‘road map’ to guide you through the process, including how to request allotments of vaccine to accommodate your patient population. View the road map here.
FDA Bans Menthol Cigarettes – Celebrate No Menthol Sunday on May 16
Last Thursday, the FDA announced it is beginning the process of banning menthol cigarettes and flavored cigars. This action is a critical step towards addressing the tobacco use epidemic and tobacco-related disparities. Read the announcement here.
Despite decades of successfully reducing tobacco use in the U.S., the progress has not been equitable. Specific populations, who have been targeted and disproportionately impacted by tobacco use, continue to use tobacco at higher rates. For example, 85-90 percent of African American cigarette smokers choose menthol flavored cigarettes, while only 30 percent of white cigarette smokers do. Studies show that mentholated cigarettes make smoking easier to start and more difficult to quit than do other cigarettes.
If implemented and equitably enforced, the FDA’s ban on menthol cigarettes and flavored cigars will keep these products off the market, and at the same time will not penalize those who purchase or possess tobacco products.
Update on Information-Blocking Rules from the 21st Century CURES Act
The regulation implementing the 21st Century CURES Act’s prohibition on information-blocking went into effect on April 5 despite the fact that many provider groups are voicing concerns that the Centers for Medicare and Medicaid Services (CMS) has not offered adequate guidance for them to determine how to comply. At present, U.S. Health and Human Services (HHS) lacks the authority to penalize health care providers for non-compliance; nonetheless, all providers will need to come into compliance with these rules at some point in the future, and doing so raises substantial legal, technical and training issues.
For more information about the new data-blocking requirements, see the following resources:
• This site has some general information: https://www.lifeimage.com/solutions/provider-exchange/onc-compliance
• The American Medical Association has issued a brief entitled “How do I comply with info blocking and where do I start?”
• HHS has extensive FAQs available here: https://www.healthit.gov/curesrule/resources/information-blocking-faqs
Reminder: there was a session at the Primary Care Conference about Information Blocking. If you registered for PCC you can still access a recording of the session through the conference website
In the News
FDA Expected To OK Pfizer Vaccine For Teens Within Week, AP News, 5-3-21
Learning Opportunity
Financing that Rewards Better Health & Well-Being Workshops -- A Free Workshop Series
May 25 | 2 to 5:30 pm
May 28 | 1 to 4:30 pm
June 2 | 2 to 5:30 pm
The discussion in this National Academy of Medicine series will address five objectives:
- Describe the deficiencies in our current health delivery and financing systems for creating health and sustaining health care delivery in light of the COVID-19 pandemic.
2. Identify and describe alternative payment models demonstrating major transformations in health care delivery and financing, address those deficiencies, and summarize their characteristics and designs.
3. Describe how integrated financing approaches can be used to redirect payment for individual services that may be unnecessary or even harmful toward payment for care of the whole person, equitable population health outcomes, improved patient and provider experience, and reduced per capita costs.
4. Evaluate how care models using integrated financing have adapted to the COVID-19 pandemic to create whole person-population health and remain financially viable.
5. Identify practical strategies and financing approaches that effectively reward whole person-population health.
Day 1 of the workshop series will focus on envisioning an integrated health care delivery and financing system.
Day 2 of the workshop series will focus on examining innovative models and levers underscored during the COVID-19 pandemic.
Day 3 of the workshop series will focus on a roadmap for integrated payment approaches to efficiency, effectiveness, and equity.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse 4-30-21
Get the latest on what has been happening at the NC General Assembly this week in this video with NCMS Director of Legislative Relations Sue Ann Forrest, MPA. As the legislative session progresses several bills we've been tracking are moving through committee including SB345 -- PA Team-based Practice, which moved through the Senate Commerce and Insurance Committee. To learn more about the NCMS' support of this legislation, be sure to tune into our webinar on Wednesday, May 5 at 6 p.m. Learn more and register here.
Other bills we continue to monitor include those on surprise billing, EPO plans and pharmacists prescribing treatments. Watch and learn more below.
NCMS Morning Rounds 4-30-21
Finally Friday! Here's your NCMS Morning Rounds.April 30, 2021Clarification: The headline in yesterday’s story about prescribing buprenorphine for opioid use disorder was misleading. The new guidelines may exempt you from certain certification requirements related to training and counseling, but an X-waiver is still required. Learn more here. A Message to YOU from NCDHHS Secretary Mandy Cohen, MD, MPHNC Department of Health and Human Services (NCDHHS) Secretary Mandy Cohen, MD, MPH speaks to primary care physicians and PAs in this video about providing the COVID-19 vaccine through your office. The goal is to make it easily accessible to as many people as possible. Watch as Sec. Cohen describes a new vaccine allocation process and how you can participate in this important effort. To get all the details, please visit the step-by-step ‘roadmap’ to enroll in the NC Vaccine Management System (CVMS) and to request vaccine once enrolled and activated. Access that roadmap here. Your Input is ImportantOver the last year the NCMS, the NC Medical Group Management Association and Curi have consistently looked to you for input on the issues facing your practice due to the COVID-19 pandemic. We have gathered important data that has helped inform policymaking and resource development. Please take just a moment to complete our latest survey. Thank you for your time and for your commitment to your communities. We’re in this together and are proud to support you and your practice through this tumultuous season. Information Blocking Regulations Begin NowThe NC Health Information Exchange Authority (NCHIEA) or HealthConnex is committed to interoperability and information sharing, and has studied and monitored the 21st Century CURES Act information blocking regulations. As of April 5, 2021, health care providers, health IT developers of certified health IT, and health information networks/health information exchanges are required to comply with the Cures Act. Additionally, health care stakeholders and participants will now benefit from more easily accessible electronic health information (EHI). Until October 5, 2021, a portion of EHI that isn’t “blocked” and limited to the data elements based on the United States Core Data for Interoperability (USCDI Version 1) will be evaluated. This evaluation period will give participants an opportunity to gain more experience and education on information blocking regulations prior to the entire regulation coming into effect, including what is required for an exception. For all technical questions about NC HealthConnex or its data-sharing capabilities, please contact the NC HIEA Provider Relations team at [email protected] or (919) 754-6912. NC HealthConnex participants can find the Request for Release of Electronic Protected Health Information form here. All updated policies, including the NC HIEA Privacy and Security Policy and User Access Policy, can be found here. In the NewsDoctors More Likely to Prescribe Opioids to Covid ‘Long Haulers,’ Raising Addiction Fears, Kaiser Health News, 4-28-21 Learning OpportunityJoin us for this free webinar: "An Insider's View of the Medical Team Task Force" Wednesday, May 5, 2021 | 6 to 7 pm Register today for what is sure to be an informative conversation. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 4-28-21
Happy Wednesday! Here's your NCMS Morning Rounds.
April 28, 2021
Get an Insider’s Perspective on the NCMS’ Medical Team Task Force’s Work
Two legislative proposals -- SB345-PA Team-based Practice, which the NCMS supports, and SB249/HB277-The SAVE Act, which we oppose, -- are being considered at the NC General Assembly this session. Both aim to modify the regulation of Advanced Practice Providers (APP), albeit in very different ways. The NCMS’ Medical Team Task Force was charged several years ago with examining the current laws regulating APPs and whether the regulations need modification.
Please join the conversation on Wednesday, May 5 at 6 p.m. when Medical Team Task Force chair, Robert ‘Charlie’ Monteiro, MD, will review the task force’s charge, the key issues it has addressed thus far and its recommendations to the NCMS Board of Directors on PA team-based care.
Register here for this free, hour-long webinar.
NCMS Joins Other Groups in Urging Ban on Flavored Tobacco Products
The NCMS has joined with public health, health equity and other groups to urge the Food and Drug Administration (FDA) to remove menthol cigarettes, flavored e-cigarettes and certain other flavored tobacco products from the market. The FDA has committed itself to respond by tomorrow, Thursday, April 29, to a citizen petition filed seven years ago calling on it to prohibit menthol flavored cigarettes.
As outlined in a letter to North Carolina’s Congressional representatives, the FDA’s Tobacco Products Scientific Advisory Committee in 2011 and the agency’s own scientific review in 2013 documented the substantial harms to public health caused by menthol cigarettes.
Tobacco use is a major contributor to four of the leading causes of death among Black Americans - heart disease, cancer, stroke and COPD. Youth e-cigarette use is another serious public health concern.
April is National Minority Health Month
During National Minority Health Month, the US Health and Human Services (HHS) Office of Minority Health (OMH) and federal and non-federal partners will focus on the impact COVID-19 is having on racial and ethnic minority and American Indian and Alaska Native communities and underscore the need for these vulnerable communities to get vaccinated as more vaccines become available. The theme for National Minority Health Month is #VaccineReady. Learn more here.
Visit the website (English | Spanish) to access resources to spread the word on social media and to sign up to receive email updates, news and activities.
In the News
Does poor sleep mean a higher dementia risk? Here's what a new study found, Advisory Board, 4-26-21
Learning Opportunity
Tobacco Free Roadmap: Resources to Help Your Organization Prepare to Be Tobacco Free, Thursday, April 29 from 9 a.m. – 4 p.m.
Beginning July 1, 2022, as part of the NC Medicaid Transformation, all physical and behavioral health facilities that contract with Medicaid must be tobacco-free. Prepare your behavioral health organization to go tobacco free.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 4-27-21
Enjoy Tuesday's NCMS Morning Rounds.
April 27, 2021
Join the Crucial COVID-19 Vaccine Effort
In order to vaccinate as many people as possible with the COVID-19 vaccine, the state now is prioritizing primary care offices as key vaccine access points. Harvard researchers estimate 17 million unvaccinated Americans will visit their primary care physician or PA in the next month, providing a great opportunity for vaccination.
“Our top priority is to make vaccines easily accessible to North Carolinians in settings they trust, so that as many people as possible are vaccinated as quickly as possible,” the NC Department of Health and Human Services (NCDHHS) said in an email sent to primary care practices last week. “Providers are encouraged to accommodate walk-in appointments and to offer vaccines as part of regular patient visits to provide the greatest flexibility and access to people wanting the vaccine. In these circumstances, getting vaccine to people who want the vaccine should be prioritized over ensuring that every dose is used in an open vial.”
To facilitate getting COVID-19 vaccine to primary care practices, the state has developed a step-by-step ‘roadmap’ to enroll in the NC Vaccine Management System (CVMS) and to request vaccine once enrolled and activated. Access that roadmap here.
Anyone age 16 and up is now eligible to receive the vaccine. Pfizer is the only vaccine currently authorized for those under age 18, but the state anticipates the Pfizer COVID-19 vaccine may be authorized for adolescents 12 and up in the next couple of weeks. Pediatric and family medicine practices please take note – if and when the Pfizer vaccine is approved for the younger age group, the state will look to you to help vaccinate 12- to 15-year-olds.
The process to become enrolled and activated to provide the vaccine in your practice can take up to two weeks. Once your practice is enrolled, you will be able to request vaccine doses for the coming week. The state is encouraging primary care practices to get started now to help in the effort to get North Carolina’s population fully vaccinated. If you need help or have questions, please reach out to your Immunization Branch Regional Nurse Consultant with the contact information listed in this map. You may also call the COVID-19 Vaccine Provider Help Center at (877) 873-6247 and select option 1 for COVID-19 questions (Monday – Friday 7 a.m. to 7 p.m. and Saturday – Sunday 10 a.m. to 6 p.m.).
Once enrolled, a new allocation process for vaccine also has been implemented in which you may request the number of first doses of vaccine for the coming week with the opportunity each week to request more doses. The previous 7-day requirement to use up all the first doses no longer exists. You may request doses on an as-needed basis, but to be considered for additional doses you should have administered at least half of your allocated vaccine. Detailed steps are outlined in the roadmap here.
NC Medicaid Payments Deadline Changes
As previously reported in this newsletter, the Advanced Medical Home (AMH) Glidepath Payment program became effective April 1. This program offers time-limited payments to practices that have attested to contacting and testing criteria as an AMH Tier 3 provider as part of the transition to NC Medicaid Managed Care. The attestation deadline for June payments has changed. To be eligible for June payments, attestation MUST be completed by May 14 at 5 p.m.
Additionally, the NC Department of Health and Human Services (NCDHHS) has developed a reconsideration process for providers who either disagree with the outcome of the validation determination for the March payment or who missed the initial attestation deadline due to COVID-19 pandemic and public health emergency related circumstances.
For more information, please see the Advanced Medical Home Tier 3 Glidepath Attestation Payment Updates Medicaid bulletin article.
CDC, FDA Lift Pause on J&J COVID-19 Vaccinations
Late last Friday, the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) lifted the 10-day pause on the Johnson & Johnson (J&J) COVID-19 vaccine after the review by the CDC’s Advisory Committee on Immunization Practices. The expert panel, in a 10-4 decision, voted to recommend vaccinations resume but with a warning label on the vaccine about the risks.
The pause in J&J vaccinations came after six cases of a rare and severe type of blood clot were reported among the 6.8 million doses of the shot administered. As of last week, a total of 15 cases of thrombosis have been reported through the Vaccine Adverse Event Reporting System. All of the cases occurred in women between ages 18 and 59, with symptom onset six to 15 days after vaccination.
During the pause, medical and scientific teams at the FDA and CDC examined available data to assess the risk of thrombosis involving the cerebral venous sinuses, or CVST (large blood vessels in the brain), and other sites in the body (including but not limited to the large blood vessels of the abdomen and the veins of the legs) along with thrombocytopenia, or low blood platelet counts. The available data suggest the chance of this occurring is very low, but the FDA and CDC will remain vigilant in continuing to investigate this risk, according to the agencies. They determined that the vaccine’s known and potential benefits outweigh its known and potential risks in individuals 18 years of age and older.
Health care providers administering the vaccine and vaccine recipients or caregivers should review the Janssen COVID-19 Vaccine Fact Sheet for Healthcare Providers Administering Vaccine (Vaccination Providers) and Fact Sheet for Recipients and Caregivers, which have been revised to include information about the risk of this syndrome, which has occurred in a very small number of people who have received the J&J COVID-19 Vaccine.
In the News
Electric Scooter Company Spin To Offer Free Rides To Charlotte Health-Care Workers, Charlotte Business Journal, 4-21-21
Learning Opportunity
Stories of resilience told by people whose lives have been impacted by the overdose crisis.
Centering lived experience is core to the work we do across the state to respond to the overdose crisis. To create a space for storytelling and sharing lived experience, the Duke Opioid Collaboratory, NC DHHS’ Injury and Violence Prevention Branch, and The Monti, will host a virtual event (using Zoom) that builds community through storytelling.
Learn more and register for this free event here.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse 4-23-21
It was another busy week at the NC General Assembly as the crossover deadline on May 14 approaches. This is when all bills filed need to have passed from one chamber to the other in order to continue being considered this legislative session. Several bills we've been monitoring moved through committee, including SB-345 -- PA Team-based Practice, which passed through the Senate Health Committee unanimously and moved on to the Commerce and Insurance Committee. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, updates you on other proposals and encourages you to take action to oppose the SAVE Act by calling your legislator. Find their contact information here.
NCMS Morning Rounds 4-23-21
Finally Friday! Here's your NCMS Morning Rounds.April 23, 2021Don’t forget today’s Power Hour! Join us at noon for a stimulating discussion on health behaviors and what health care professionals can do to ensure clear communication with patients as well as underlying assumptions vs. patient understanding and the importance of building trust. Participants will also touch on the current pandemic and its impact on health behaviors. Register here for what is sure to be a lively conversation. Efforts to Get Everyone Vaccinated Against COVID-19At both at state and national levels officials are pushing to get everyone vaccinated to help stop the devastation wrought by COVID-19. One group that may be challenging to vaccinate is seniors who are homebound. This article made me think about the members of my church who are homebound. This article details some of those challenges. To help ensure this group has access to the vaccine, the NC Department of Health and Human Services (NCDHHS) has a list of who will provide in-home vaccination to housebound people listed by county. Access this useful resource here. Also, be sure to get the latest on vaccinating your patients in an upcoming webinar, Tuesday, April 27 at 6 p.m. ‘Navigating Ahead- Vaccinating Your Patients for COVID-19’ is co-sponsored by NCAFP, the NC Pediatric Society, the NC Psychiatric Association, the NC AHEC Program and Community Care of North Carolina. Now that the vaccine-eligible population has grown to all adults and a childhood vaccine is on the horizon, more and more medical practices are or will be administering vaccines, either in partnership with others or in their own offices. Hear from your colleagues who are thinking through the “nuts and bolts” of patient vaccinations. You can join the Zoom meeting by clicking here or dial in at 646-558-8656 using webinar ID 131 899 801. Progress is being made in vaccinating our population in North Carolina. More than 100,000 doses of COVID-19 vaccine have been administered through the federally supported vaccination center that opened March 10, 2021 in Greensboro. The Greensboro clinic will be extended through May 27 and will continue to provide the Pfizer vaccine. While appointments are encouraged and available online at GSOmassvax.org or by phone at 888-675-4567, walk-in and drive-up vaccines are also available without appointment. Guilford County was selected for a vaccination site by FEMA and the CDC as an area with significant underserved or marginalized populations. The site is organized and operated by the state and staffed through the U.S. Department of Defense. It is supported with resources from Guilford County, the North Carolina Department of Public Safety, including the Division of Emergency Management and the North Carolina National Guard, and NCDHHS. NCMS President Has New PositionNovant Health recently announced several leadership updates as its integration with New Hanover Regional Medical Center (NHRMC) continues. Effective May 1, current NCMS President Philip Brown, Jr., MD, will be the system’s chief community impact officer. In this role, as part of the Novant Health diversity, inclusion and equity team, Dr. Brown will be charged with engaging the community in advancing health equity. He was previously the executive vice president and chief physician executive at NHRMC. Congratulations, Dr. Brown! Get a Start on Your Summer Reading with the NCMS Book ClubBelieve it or not, summer--and therefore, summer reading--is just around the corner! We would love to have you join our NC Medical Society Book Club and connect with your colleagues via stimulating discussions on exciting books. From late May through the end of July, we will be reading The New York Times bestselling memoir The Beauty in Breaking: A Memoir by emergency department physician Michele Harper. Harper tells the poignant true story of her journey toward self-healing. Each of the patients Harper writes about taught her something important about recuperation and recovery; how to let go of fear even when the future is murky and how to tell the truth when it's simpler to overlook it. Our book club connects through a private online forum for participants to discuss books and learn from one another. We spend about 10 weeks on each book, so there is always plenty of time to read each book! Sign up and learn more about our next book here! In the NewsFDA: Make Medical Apps Reliable, Not Risky, STAT News, 4-21-21 Learning OpportunityThe Road to Equity: Examining Structural Racism in Health Care, Tuesday, April 27, 1 – 4:30 p.m. and Wednesday, April 28, 1 – 4:45 p.m. Learn more and register for Day 1 here. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 4-22-21
It's Thursday and time for your NCMS Morning Rounds.
April 22, 2021
Dr. Crockett speaks at Tuesday's press conference at the NC General Assembly.
NCMS, NC ObGyn Society Support Dignity for Incarcerated Women Proposal
On Tuesday the NCMS and NC Obstetrical and Gynecological Society (NCOGS) issued a joint media statement in support of NC House Bill 608 -- Dignity for Women Who Are Incarcerated. This legislative proposal, introduced on Tuesday, addresses the health needs of incarcerated women and their babies by codifying standards of care for women’s health and perinatal care.
Rep. Kristen Baker, MD (R-Cabarrus), the only physician in the NC General Assembly, is one of the bill’s co-sponsors. At a press conference held at the General Assembly just after the bill was filed, Rep. Baker and the co-sponsors were joined by Kerianne Crockett, MD, a Greenville Obstetrician-Gynecologist and NCOGS board member, who spoke emotionally about one of her patients.
“Nearly two years ago I took care of a patient who was in detention at an area jail during her pregnancy. She was restrained with ankle and wrist cuffs during her labor, delivery, part of her post-partum time. She also suffered the devastating loss of her infant,” she said. “In the months that followed, I grappled with my own grief over her loss and thought nonstop about how her difficult and heartbreaking experience was turned into a traumatic one by the shackles she was forced to wear.”
The proposed legislation would protect the health and safety of mother and baby by prohibiting shackling of pregnant women in the second and third trimesters, during labor and delivery and allowing only limited restraint for six weeks post-partum. Also, the bill insists mothers receive adequate nutrition to support their baby’s health and welfare.
Read the NCMS’ and NCOGS’ media statement here.
Improved Communication Access Pilot Project
The NC Division of Services for the Deaf and Hard of Hearing (DSDHH) has partnered with the NC Division of Health Benefits to establish a pilot initiative to improve access to communication services for deaf, blind and hard of hearing patients – and their companions – who have Medicaid and Health Choice.
One reason many medical practices are resistant to providing communication accommodations is the cost related to these services. Through this initiative, practices can register to be reimbursed for communication access services such as American Sign Language (ASL) interpreters and Communication Access Real-time Translation (CART). Register here.
Examples of visits covered are medical appointments, eye exams, in-home health care, mental health counseling sessions and more.
Learn more about this initiative here.
For more information about this pilot service, please reach out to the Medicaid Communication Access Coordinator at [email protected] or (984) 884-1093.
More Telehealth Funding Available
The Federal Communications Commission (FCC) recently announced that applications for Round 2 of funding for the COVID-19 Telehealth Program will be accepted beginning on April 29 and ending on May 6. The $249.95 million federal initiative builds on the $200 million program established as part of the CARES Act.
You can learn more about this funding opportunity in a webinar this Friday, April 23 at 1 p.m. Access the webinar at this Zoom link.
Community Health Centers are encouraged to consider applying.
- The application will be fairly simple. Applicants must provide some basic data, but no extensive narratives are required.
• Given the scoring system that the FCC has established, community health centers are well-positioned to be approved for funding – particularly those who applied in Round One (last spring/ summer) but were not funded.
• Applicants can receive up to $1 million to support 100 percent of the cost of services and supplies needed to expand telehealth.
Learn more about this opportunity here.
In the News
New Coronavirus Variant Found In Texas, Becker’s Hospital Review, 4-20-21
Learning Opportunity
Priorities on the Health Horizon: Informing PCORI's Strategic Plan Webinar, April 27 | 11 am – 2 pm
The meeting will be anchored by two compelling, forward-looking questions:
-What will it take to create a patient-centered learning health system (with respect to infrastructure, technologies, and engagement)?
-How can PCORI use its research strategies, unique role, and activities to improve patient experience, outcomes, and value in health and health care?
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Political Pulse for April 16, 2021
Even though the NC General Assembly was on their spring break last week, many bills were filed especially in the Senate to meet the filing deadline. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA describes some of the proposals introduced including a bill giving pharmacists authority to prescribe certain medications, several bills concerning medical liability, proposed legislation that would extend the mandatory deadline to connect to the state's Health Information Exchange (HIE) and a slew of public health focused proposals. For a comprehensive list of all the many bills we're tracking, please visit our Legislative blog here.
And please use our Action Alert, if you haven't already, and encourage your colleagues to use it to let legislators know about our opposition to SB249/HB277 -- the SAVE Act. Here is the link to that alert.
NCMS Morning Rounds 4-16-21
Friday and your NCMS Morning Rounds have arrived!April 16, 2021Navigating COVID-19 Vaccination EffortsThe Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP) held an emergency meeting Wednesday to look more closely at the thromboembolic events associated with the Johnson & Johnson (Janssen) COVID-19 vaccine. Review the presentations and updates from that meeting here. The committee did not make a recommendation, indicating they will continue to assess the data and risks and will reconvene in a week to 10 days. In the meantime, the CDC’s and Food and Drug Administration’s (FDA) recommended pause in the administration of the J&J vaccine will continue. North Carolina officials suspended use of the J&J vaccine earlier this week. American Medical Association President, Susan R. Bailey, MD, recently hosted a webinar with Peter Marks, MD, PhD, Director of the Center for Biologics Evaluation and Research at the FDA. The conversation focused on the Johnson & Johnson (Janssen) vaccine. View the webinar at this link. In North Carolina, health care practices continue to combat vaccine hesitancy, strive for equity in vaccine administration and address the logistics of ensuring everyone in the community is vaccinated against COVID-19. On Tuesday, April 27 at 6 p.m. NC AHEC is bringing together physicians who are in the thick of this effort to share their experiences in getting their patients vaccinated. Speakers include Garett Franklin, MD, Cary Medical Group/Raleigh Medical Group, Greg Adams, MD, Blue Ridge Pediatric and Adolescent Medicine in Watauga County and Rasheeda Monroe, MD. Click here to Join the Zoom meeting room on your computer, or dial-in at (646) 558-8656 using webinar ID 131 899 801. Kanof Institute for Physician Leadership Now Accepting ApplicationsThe NCMS Foundation’s Kanof Institute for Physician Leadership is now accepting applications for its 2022 classes of scholars for its Leadership College and Health Care Leadership and Management programs. The application deadline is June 30. If you would like to learn more about these programs, please submit an interest form (see below) or email Aubrey Cuthbertson at [email protected]. Submit a Leadership College interest form here. Submit a Health Care Leadership and Management interest form here. Learn more about the Kanof Institute for Physician Leadership and all its programs. Project OBOT Supporters Receive Glaser AwardBlake Fagan, MD, and Eric Morse, MD were both recently awarded the Frederick B. Glaser Award at the Addiction Medicine 2021 conference. The biennial award, given by the Governor’s Institute and the NC Chapter of the American Society of Addiction Medicine (ASAM), honors addiction medicine physicians for achievement and meritorious service in the domains of substance use disorder treatment, education, research and leadership. Dr. Fagan, a family physician at the Mountain Area Health Education Center (MAHEC) in Asheville and a professor in the Department of Family Medicine at UNC-Chapel Hill, has served as the co-director of the Office-Based Opioid Treatment (OBOT) services provided at MAHEC’s Family Health Center since its inception in 2015. He is part of the NCMS’ Opioid Task Force and supportive of the NCMS Foundation’s Project OBOT. Dr. Morse, an addiction and sports psychiatrist, is the medical director for two Opioid Treatment Programs (OTPs) and a program physician at five Morse Clinics across the Triangle. Both physicians have been pivotal in increasing access to medication assisted treatment for opioid use disorder in NC through extensive training, mentoring and technical assistance to other physicians and advanced practice providers. Congratulations Drs. Fagan and Morse! In the NewsThe US Paused Use of J&J's Vaccine. What Happens Next? Health Care Dive, 4-14-21 Learning OpportunityNavigating Ahead on Vaccinating Your Patients with COVID Vax, Tuesday, April 27 | 6–7 PM Come hear from your colleagues who are thinking through the “nuts and bolts” of patient vaccinations. Join meeting here. Or dial in at (646) 558-8656 using webinar ID 131 899 801. If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 4-14-21
Enjoy your mid-week NCMS Morning Rounds.April 14, 2021CDC and FDA Recommend Pause in Administration of J & J COVID-19 VaccineOn Tuesday, the NC Department of Health and Human Services (NCDHHS) announced it will follow the recommendation of the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) to suspend administration of the Johnson & Johnson (Janssen) COVID-19 vaccine. The CDC and FDA are reviewing data involving six reported US cases of a rare and severe type of blood clot in individuals after receiving the J&J vaccine. The type of blood clot, a cerebral venous sinus thrombosis, was seen in combination with low levels of blood platelets. The six cases occurred in women between ages 18 and 48 with symptoms occurring six to 13 days after vaccination. Treatment of this specific type of blood clot is different from the treatment that might typically be administered. Usually, an anticoagulant drug called heparin is used to treat blood clots. In this setting, administration of heparin may be dangerous, and alternative treatments need to be given, according to the CDC and FDA. It is important for the health care provider community to be aware of the potential for these adverse events and can plan for proper recognition and management due to the unique treatment required with this type of blood clot. Right now, these adverse events appear to be extremely rare. People who have received the J&J vaccine who develop severe headache, abdominal pain, leg pain or shortness of breath within three weeks after vaccination should contact their health care provider. Health care providers are asked to report adverse events to the Vaccine Adverse Event Reporting System here. Today the CDC will convene a meeting of the Advisory Committee on Immunization Practices (ACIP) to further review these cases and assess their potential significance. FDA will review that analysis as it also investigates these cases. Until that process is complete, these federal agencies are recommending a pause in the use of this vaccine out of an abundance of caution. You can watch a videotaped media briefing with officials from the CDC and FDA as they brief reporters and answer questions about their recommendation here. As of Monday, more than 6.8 million people in the US have received the J&J vaccine, while about 98 million people have received the Pfizer vaccine and 85 million the Moderna vaccine. According to the CDC, about 9 million J&J shots have been distributed, but are now on hold due to the CDC’s and FDA’s recommendation. NCMS Foundation’s Our Community Health Initiative Has New PartnerThe NCMS Foundation’s Our Community Health Initiative (OCHI) has announced a new partnership with IndividuALLytics to provide remote patient monitoring and behavioral health integration for comprehensive chronic care management, leveraging the company’s precision medicine model. "We are pleased that IndividuALLytics is joining our team, which will enhance the scope and scale of services provided by OCHI," said NCMS Vice President for Rural Health Systems Innovation Franklin Walker, MBA. OCHI offers medical practices a way to seamlessly collaborate with and connect patients to community based organizations providing services that improve health. For instance, OCHI offers a referral platform in which physicians and PAs can easily refer patients to evidence-based diabetes prevention programs and others offered through the YMCA in communities throughout the state. “OCHI has done a great job making it easier for organizations like the YMCA to manage Diabetes Prevention Programs,” Walker said. “Our success with OCHI has allowed us to engage the assistance of the American Medical Association to expand and share this simple to use platform nationally.” “IndividuALLytics offers our community-based organizations and health provider customers additional expertise in deploying and managing state of the art data collection processes, including physical, biometric and disease specific, which increases the physician’s ability to manage care,” according to Reynold Yordy, founder and Chief Technology Officer for IndividuALLytics. Michigan-based IndividuALLytics, Inc. employs patent-pending individualized N-of-1 treatment protocols for precision management of chronic illness and employs a comprehensive solution for remote patient monitoring along with a mobile application for patient engagement and multidisciplinary virtual care teams to determine and administer these individualized treatment protocols. OCHI, part of the NCMS Foundation, uses a software platform that provides custom EHR functionality to community-based organizations allowing them to participate in a collaborative and integrated approach to health. The program enables individual and group interactions, whether face-to-face or virtual, to assist in managing individual care plans. OCHI enables physicians and PAs and community-based organizations to collect and digitally exchange relevant data with the expectation of demonstrating positive health outcomes. Learn more about OCHI. Resources to Encourage NC Medicaid EnrollmentThe NC Department of Health and Human Services (NCDHHS) has launched a public messaging campaign to encourage Medicaid beneficiaries to enroll in NC Medicaid Managed Care. The “Choose Your Path to Better Health” campaign includes a variety of television and radio spots that are airing in English and Spanish as well as internet and social media messages. NC Medicaid community partners, advocates, health care providers and other stakeholders may use these materials to help share the word about NC Medicaid Managed Care and the open enrollment period, which runs through May 14. This toolkit includes the advertising listed above plus digital images and flyers that can be printed and posted. In addition to the Choose Your Path campaign, NC Medicaid is promoting the enrollment period using social media posts, community webinars and events, as well as a prior press release and a Medicaid bulletin. In the NewsFully Vaccinated But COVID-19 Positive? 4 Notes On Breakthrough Case Prevalence, Becker’s Hospital Review, 4-12-21 Learning OpportunityDiabetes Prevention & Best Practices Learning Collaborative (LC) If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 4-13-21
Happy Tuesday! Enjoy your NCMS Morning Rounds.
April 13, 2021
TODAY: Learn More About Reimbursement for Treating COVID-19 Uninsured
Today, Tuesday, April 13 at 2 p.m. the Health Resources and Service Administration (HRSA) is offering a webinar for you to learn more about the HRSA COVID-19 Uninsured Program. Participating providers are reimbursed at Medicare rates for testing, treating and administering COVID-19 vaccines to uninsured individuals.
If you have conducted COVID-19 testing to uninsured individuals, provided treatment for uninsured individuals with a COVID-19 diagnosis on or after February 4, 2020, or administered COVID-19 vaccines to uninsured individuals you can begin the process to file claims for reimbursement.
Familiarize yourself with this process here, and learn more and file claims here. You can also view Frequently Asked Questions about the program.
And join HRSA officials today at 2 p.m. to learn more. Register here for the webinar.
CDC Declares Racism Serious Public Health Threat
Last week the Director of the Centers for Disease Control and Prevention (CDC) Rochelle P. Walensky MD, MPH, declared racism a serious public health threat. Read her public statement here.
In her remarks she also highlighted the CDC’s new website, ‘Racism and Health,’ which will serve as the hub for the agency’s efforts to combat this public health threat and serve as a catalyst for greater education and dialogue around this critical issue. The webpage contains information on structural racism, social determinants of health and their impact on health outcomes in communities of color. Access the website here.
NC Academy of Family Physicians Podcast Focuses on Diabetes Prevention
The latest episode of NCFM Today, the NC Academy of Family Physicians podcast hosted by NCAFP Executive Vice President Greg Griggs, MPA, CAE, features NCMS Board member and DiabetesFreeNC physician champion Karen Smith, MD, and NCMS Vice President for Rural Health Systems Innovation Franklin Walker, MBA.
Dr. Smith, a family physician in Raeford, NC, describes how she screens patients and refers them to one of our state's Diabetes Prevention Programs. Walker talks about how physicians can get involved in the Diabetes Free NC initiative, part of a wide-ranging coalition of organizations including the NCMS Foundation and the AMA. Learn more here.
Listen to the 18-minute podcast here.
In the News
Scientists Work Toward An Elusive Dream: A Simple Pill To Treat Covid-19, STAT News, 4-9-21
Learning Opportunity
Enhancing Knowledge and Skills in Adult Mental Health, April 29, 2021 9:15 AM - April 30, 2021 4:45 PM
Part of this conference will focus on the impact of COVID-19 on the behavioral health system and on individuals of color. It will reflect on the grief and loss we have all experienced and continue to experience since the pandemic began. Our keynote speaker, Dr. Sy Saeed, Chair of the Department of Psychiatry and Behavioral Medicine at East Carolina University, will outline the impact of COVID on our mind and body, the magnitude of our current behavioral health workforce shortage, and the benefit of telepsychiatry in addressing these issues. We will also offer sessions that focus on whole person care, psychopharmacology, cultural diversity focusing on Latinx and African American clients, mental health literacy and the stigma of mental illness, PTSD, and use of cannabis in treating mental illness. Nursing credit offered - target audience is psychiatric, substance use, and advanced practice nurses and nurse practitioners.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 4-12-21
Welcome to a new week of NCMS Morning Rounds.April 11, 2021Key Differences Between PA Team-Based Practice and SAVE Act ProposalsTo help clarify the differences between the two proposals currently being considered by the NC General Assembly around PAs and advance practice nurses, the NCMS has developed a side-by-side comparison chart to clearly distinguish the content of SB345 – Physician Assistant Team-based Practice and SB249/HB277—The SAVE Act. We also are in the process of developing a comprehensive FAQ document to address your questions and concerns about these proposals, the current statutes as well as the NCMS’ policies on scope of practice and team-based settings. Stated broadly, the most important differences between these bills are: SB249/HB277—The SAVE Act, which the NCMS opposes, completely removes required supervision in all circumstances regardless of practice setting and/or clinical experience. For a more detailed comparison access the comparison chart here. PPE AND COVID-19 Tests Available through the NCMSJust a reminder that the NCMS is still offering personal protective equipment (PPE) for purchase through our ActionPPE supplier. You can shop conveniently online at this link on the NCMS website. PPE available includes gowns, face shields, gloves and a variety of masks. In addition, the NCMS is partnering with ActionPPE, which has negotiated a special group buy on FDA approved Covid Rapid Antigen Tests. These test, which can be done in a provider’s office in just 10 minutes, are being offered at below market prices. This is a one-time group purchase of 100k American-made COVID Antigen Test Kits for medical professionals only. Reserve your Covid test kits today as stock will be allocated on a first-come-first-serve basis. Remember to use your NCMS discount code: NCMS-SAVE5. Order now. Getting Ready for Medicaid TransformationWith the warmer weather the series of webinars on the state’s move to Medicaid managed care are now being called ‘Back Porch’ chats rather than ‘fireside’ chats. The next in the series, which is presented by the NC Department of Health and Human Services (NCDHHS) in partnership with NCAHEC, will happen this Thursday, April 15 from 5:30 to 6:30 p.m. and will address a variety of hot topics around the launch of Medicaid managed care, which will happen on July 1. To generally stay up to date on this massive shift, be sure to read the most recent NC Medicaid Bulletins at the Bulletin webpage here. Some of the latest issues cover: • New and Amended Clinical Coverage Policies – March 2021 In the NewsYounger Healthcare Workers Especially Stressed By COVID-19, Poll Finds, Becker’s Hospital Review, 4-6-21 Learning OpportunityJoin us for the next free Lunch and Learn Webinar: "Diabetes Prevention Program", Tuesday, April 20 | noon to 1:00 pm If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
|
NCMS Morning Rounds 4-8-21
Enjoy Thursday's NCMS Morning Rounds. April 8, 2021
Don’t forget tomorrow’s (Friday, April 9) Power Hour beginning at noon. Our guests will focus on black maternal health.
Health inequity in the US has become more apparent during the pandemic, with COVID-19 disproportionately ravaging populations of color. Statistics confirm similar health outcomes for this population in other areas like maternal health. The US has the worst maternal mortality rates overall compared to other developed countries, with black mothers at least three times more likely to die in childbirth than white mothers. Black babies have a mortality rate almost four times the rate of their non-Hispanic white counterparts.
Join us as we hear what some of our community members are seeing in this area and what actions are being taken to address and improve the health outcomes for black mothers.
COVID-19 Testing Pilot Program Underway
The North Carolina Department of Health and Human Services (NCDHHS), in partnership with Labcorp, is piloting a program to provide 35,000 no-cost, home test collection kits to North Carolinians receiving Food and Nutrition Services and/or are disabled and experiencing barriers to getting tested.
Eligible North Carolina residents can request a Pixel by Labcorp™ COVID-19 PCR Test Home Collection Kit be shipped overnight directly to their homes. The test kit includes test supplies (nasal swab, sample container, etc.), detailed instructions and prepaid specimen return shipping materials to make mailing samples back to Labcorp for testing easy and convenient. Results are typically reported back to the individual within 24 to 48 hours from the time the specimen is received at the lab. Once processed by Labcorp, test results are accessed by the customer via the Pixel by Labcorp website.
The program’s initial pilot is designed to provide testing resources to individuals with symptoms of COVID-19 or who may have been exposed and are members of the following eligible populations:
• Beneficiaries of North Carolina Food and Nutrition Services (formerly called the Food Stamp Program), who may have difficulty accessing existing state-funded testing sites and resources
• Persons with disabilities such as cognitive/intellectual, physical and sensory, substance abuse, mental health and other disabilities that impact their ability to access COVID-19 testing sites
It’s Not Too Late -- Join the NCMS Book Club and Meet With Matt Haig!
The NCMS Book Club is currently reading the international best-seller The Midnight Library. We would love to have you join us for our current reading period culminating in a live, exclusive Q&A session with in-demand author Matt Haig!
There is no cost to participate in this club -- you just need a copy of the book to enjoy. Book club members connect through a private online forum where participants discuss the book and learn from one another. Our book club will spend about 10 weeks on each book, so you'll have plenty of time to read. Sign up here.
If you are not yet a book club member, sign up now so you can participate in what is sure to be an interesting conversation about what led Haig to write The Midnight Library and to ask him your burning questions. If you’re already a club member, you should have received the registration link to this exclusive event in your email.
Curi Acquires Health Care Data Analytics Company
Curi, which provides professional liability and other lines of insurance, wealth management and advisory services to physicians, announced that it has acquired the health care data analytics and advisory company, Arrowlytics. Building on an existing five-year relationship between the two organizations, the acquisition will strengthen Curi’s suite of advisory services for physicians and their practices by adding a data-driven solution to help their businesses thrive.
Arrowlytics’ Aspire platform pulls critical data from disparate sources into one system, allowing practices to monitor and improve results across a variety of performance categories—from online reputation management, to practice growth and optimization. Coupled with consultative support from a team of seasoned health care industry experts from both Arrowlytics and Curi, the solution will allow practice leaders to make more informed decisions to assess, adjust and ultimately grow their business.
“Running a medical practice gets more challenging every year, and we have been proud to help our member physicians and their practices navigate these challenges for more than four decades,” said incoming Curi CEO and NCMS Foundation Trustee Jason Sandner. “At Curi, we are always looking for new ways to support our members, and bringing the team and solutions from Arrowlytics into the Curi family will allow us to offer new data-centered solutions and services to the healthcare leaders that we serve.”
The Arrowlytics Aspire platform will support the advisory products and services that Curi has been actively developing with input from its member community for years—from enhancements to risk management, to health policy guidance, to practice retirement plan solutions, to well-being offerings, and more. The offering will be especially valuable in light of the numerous financial and operational challenges that practices are facing during this period of transition in service delivery models.
In the News
Will Vaccines Roll Out In Time To Stop Emerging Variants? Here's What Experts Say, Advisory Board, 4-6-21
Learning Opportunity
2021 Virtual Primary Care Conference, April 7 @ 8 am - April 9 @ 5 pm
Conference tracks will cover areas including: billing and coding, clinical, executive leadership development, and care management, with sessions dedicated to COVID, social determinants of health, and diabetes care.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!
NCMS Morning Rounds 4-5-21
Happy Monday! Enjoy your NCMS Morning Rounds.
April 5, 2021
NCMS Legislative Update
This week is ‘spring break’ for legislators, who last week were hurrying to file bills before heading out of town.
While legislators were focused on two education bills being pushed by House and Senate leadership on summer school and reading for the state’s children, other bills of note for physicians and PAs deserve special mention.
As mentioned previously, SB345 – PA Team-based Practice is a proposal that modernizes how physicians supervise PAs, recognizing training and education and focusing on team-based care. The NCMS supports this legislation, which is a product of the NCMS’ Medical Team Task Force’s work over two years. The NCMS joined the NC Academy of Physician Assistants in issuing a media statement when this bill was introduced. Read that statement here.
NCMS staff also is developing an FAQ document outlining the Task Force’s formation and charge as well to answer your questions about the legislative proposal. Watch your NCMS Morning Rounds for this document. In the meantime, please email any questions you have to [email protected] so we can respond to you and include the answers in our FAQ document, which will be updated frequently.
HB61 – Local Communicable Disease Programs/Funds, which provides additional state funding to health departments to fight COVID-19 as well as other infectious diseases. This bill has moved on to the House Appropriations committee for consideration.
The first proposal dealing with surprise billing was filed last week. SB415—Greater Transparency in Health Care Billing was introduced and we will be monitoring it closely.
SB486 – Reform Courts and Jails is an extremely lengthy bill, but included in it is a provision of particular interest to obstetricians and gynecologists on shackling pregnant women who are incarcerated.
SB255 – 2021 AOC Legislative Changes includes provisions that could impact medical liability. We are closely watching this proposal.
Please visit our NCMS legislative blog for daily updates on action at the NC General Assembly. This will be a quiet week as legislators enjoy their break, but get ready for busy weeks ahead as bill filing deadlines approach and the budget negotiations begin.
Tax Season is Here –NCMS Dues Deductibility Statement
Federal law requires the NCMS to notify members that a percentage of dues paid by members is not deductible in accordance with IRC section 6033 regarding professional dues. Dues to the NCMS and component societies are not deductible as charitable contributions for federal income tax purposes but a portion may be claimed as a business expense.
For tax year 2020 it is estimated that 14 percent of NCMS dues is non-deductible. Component societies deductibility amounts for 2020 are as follows:
• NC Dermatology Association: 100 percent non-deductible
• NC OBGYN Society: 28 percent non-deductible
• NC Orthopaedic Association: 48 percent non-deductible
• NC Society of Eye Physicians & Surgeons: 69 percent non-deductible
For 2021 it is estimated that 12 percent of the 2021 NCMS dues amount paid by members is not deductible with IRC section 6033 regarding professional dues.
If you made charitable contributions to the NCMS Foundation (thank you!), you can review your giving history on your NCMS profile page. If you have already created a profile, simply go to the membership tab at the top of our homepage (www.ncmedsoc.org) and click on ‘My Homepage’ where you’ll find a link to ‘View My Giving History.’
If you do not have an NCMS profile, we encourage you to create one – it’s simple, quick and will help you manage your NCMS account. Just go to ‘login’ in the black bar at the top of our homepage or click on this link: https://www2.ncmedsoc.org/login. Follow the prompts to create your profile and access information about your NCMS membership and giving anytime.
Friday’s Power Hour Focuses on Black Maternal Health
Please join us this Friday, April 9 at noon when our NCMS Foundation Kanof Institute for Physician Leadership virtual Power Hour will focus on black maternal health.
Health inequity in the US has become more apparent during the pandemic, with COVID-19 disproportionately ravaging populations of color. Statistics confirm similar health outcomes for this population in other areas like maternal health. The US has the worst maternal mortality rates overall compared to other developed countries, with black mothers at least three times more likely to die in childbirth than white mothers. Black babies have a mortality rate almost four times the rate of their non-Hispanic white counterparts.
Earlier this year, democratic Sens. Alma Adams (NC), Michael Bennet (CO) and Corey Booker (NJ) introduced the Black Maternal Momnibus Act of 2021, which includes 12 provisions addressing racial and ethnic disparities aimed at better outcomes for – and saving the lives of -- black mothers and their children. Join us as we hear what some of our community members are seeing in this area and what actions are being taken to address and improve the health outcomes for black mothers.
In the News
'More confidence about the results': FDA authorizes two rapid coronavirus tests for home screening, USA Today, 4-1-21
Learning Opportunity
Xavier University of Louisiana's Virtual Health Disparities Conference, April 7 - 8
Look forward to:
• Award-Based Student Poster Competition (Abstracts)
• An Engaging and Interactive Town Hall Meeting
• 6th Annual John Ruffin Lecture
• Valuable networking opportunities
NCMS Political Pulse for April 2, 2021
With legislators looking forward to their 'spring break' next week, there were a flurry of bills filed this week. Watch as NCMS Director of Legislative Relations Sue Ann Forrest, MPA, highlights several that are of particular interest to physicians and PAs, including SB345-PA Team-based Practice; the first bill focused on surprise billing and several that could impact medical liability. For a daily update and summaries of all the legislation filed that we are monitoring, please visit our NCMS legislative blog.
NCMS Morning Rounds 3-31-21
Welcome to Wednesday's NCMS Morning Rounds.
March 31, 2021
Doctors’ Day Special Recognition
Leading up to yesterday’s Doctors’ Day celebration of all you do, the NCMS Foundation offered a chance to extend special recognition to individual physicians by donating $10 to the Foundation in their honor. Thank you to the generous donors who felt moved to publicly pay tribute to the following individuals. And thank you once again for all you do for your patients each and every day!
Adeel Siddiqui, MD
Terry Grant, MD
Gary O. Bean, MD
Bill Ferrell, MD
Rachel Keever, MD
Katie Lowry, MD
Lyndon Jordan, MD
Connette McMahon, MD
Josiah Duke, MD
Christopher Hasty, MD
Philip Perdue, MD
Christopher Barsanti, MD
Michelle Jones, MD
Jennie Byrne, MD, PhD
Darlene Menscer, MD
Tracy Eskra, MD
Karen Smith, MD
Dana Chambers, MD
Eileen Raynor, MD
Rachel Keever, MD
Holly Biola, MD
Danielle Mahaffey, MD
Joseph Pinkerton, MD
NCMS Leadership Development Programs Recruiting Now
The NCMS Foundation’s Kanof Institute for Physician Leadership currently is recruiting fr two of its programs – Leadership College and Health Care Leadership and Management. Both programs are project-based and focus on developing authentic leadership. That means alumni of the programs have looked inward to examine their own strengths and weaknesses as leaders to understand how to be most effective in driving positive change as part of the larger health care team as well as in the broader community.
The Institute’s foundational Leadership College delves into an individual’s leadership development. Each participant works on a year-long project involving a real-world issue where they can demonstrate their newly acquired leadership insights. At the culmination of the program each scholar summarizes their research findings in a TEDTalk-style presentation we call MEDTalks. You can watch the wide variety of previous years’ presentations here.
Learn more about and apply for Leadership College here.
The Health Care Leadership and Management track has a finance and management component as well as leadership development focus. This year-long course places special emphasis on deeper leadership development and skills that include strategic planning, negotiation and financial literacy and application.
Learn more about and apply for Health Care Leadership and Management here.
Both programs boast small class sizes with lots of personal attention and interaction with faculty and colleagues. The courses went virtual during the pandemic but are now moving toward a hybrid of virtual and in-person sessions.
Interested in hearing from alumni about their Kanof Institute experiences? The Summer 2020 issue of the NCMS Bulletin online magazine features a variety of Kanof Institute alumni recounting their ‘leadership journeys,’ and how the programs helped them each define what leadership means to them and how they currently are using the skills they gained. Read these profiles here.
If you have any questions about the programs, please contact Aubrey Cuthbertson [email protected].
Please Help Us Track COVID-19 Trends
Since the beginning of the pandemic last March, the NCMS, NC Medical Group Management Association and Curi have regularly surveyed our membership on issues they are experiencing due to the pandemic. Over time this information has helped inform our advocacy and resource development on your behalf.
Please take a moment to help us to continue to assess the impact on your practice of the COVID-19 pandemic by taking this week’s survey.
Read a summary of the key takeaways from 2020 here.
In the News
Senate Reaches Deal To Extend Medicare Pay Bump For Health Care Providers Through 2021, STAT News, 3-23-21
Learning Opportunity
Eliminate Tobacco Use Summit 2021, Wed and Thurs, April 14-15
The Eliminate Tobacco Use Initiative convenes an annual summit addressing the key areas of policy, prevention/education and cessation.
If you have policies you'd like your NCMS Board of Directors to consider, please complete the Board input form here. Thanks for reading!